Case Study
Introduction:
Necrotizing fasciitis (NF), commonly known as flesh-eating disease, is an infection that results in the death of parts of the body’s soft tissue (1). Necrotizing fasciitis is most commonly caused by an infection with group A Streptococcus (5). It is a severe disease of sudden onset that spreads rapidly (1). Symptoms include red or purple skin in the affected area, severe pain, fever, and vomiting (1). The most commonly affected areas are the limbs and perineum (2). Risk factors include poor immune function such as from diabetes or cancer, obesity, alcoholism, intravenous drug use, and peripheral artery disease (2),(1). In addition to looking at patient’s skin, doctor may perform several tests to diagnose this condition. They may take a biopsy, which is a small sample of the affected skin tissue for examination (5).In other cases, blood tests, CT, or MRI scans may help doctor make a diagnosis. Blood tests can show if your muscles have been damaged (5).It is usually treated with surgery to remove the infected tissue, and intravenous antibiotics (2),(1). Necrotizing fasciitis occurs in about 0.4 people per 100,000 per year in the US, and about 1 per 100,000 in Western Europe (3). Both sexes are affected equally (2). It becomes more common among older people and is rare in children (3). The term “necrotizing fasciitis” first came into use in 1952 (3), (4).
Necrotizing Fasciitis’s Management Objectives:
The treatment for Necrotizing Fasciitis involves the principles of treatment for any kind of surgical infection (6):
- Source control (Debridement & contentious cleansing/ irrigation).
- Antimicrobial therapy.
- Organs support (Nutritional support, fluids resuscitation, blood component therapy.)
- Monitoring in an intensive care setting
Source Control:
Early recognition and prompt aggressive debridement of all necrotic tissue are needed in addition to intravenous broad-spectrum antibiotics and analgesia (7).
Topical irrigation solution has also been used extensively for wound bed cleansing, debris and exudate removal, and microbial eradication. NPWT with instillation (NPWTi) combines the use of NPWT with a topical irrigation solution. The use of NPWT used in conjunction with instillation provides an important evolution in the NPWT concept with the potential added benefit of supplying an antimicrobial solution to the wound bed (8).
The concepts of suction and wound irrigation are a longstanding principle of surgery. Fleischmann et al in 1998 reported a gravity-fed intermittent instillation system used in conjunction with NPWT (9).
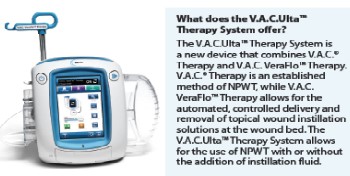
In 2003, the first commercially available NPWT device with intermittent installation was introduced (V.A.C. Instill Wound Therapy System, Kinetic Concepts Inc, San Antonio, TX) (8). the next generation of NPWT devices with instillation was introduced and since has rapidly gained popularity (V.A.C. Ulta Wound Therapy System, Kinetic Concepts Inc, San Antonio, TX; Quantum, Innovative Therapies Inc, Gaithersburg, MD) (8).
The V.A.C.Ulta™ System is an integrated negative pressure wound therapy (NPWT) system that o!ers standard NPWT (V.A.C.®Therapy) and an instillation option using V.A.C. VeraFlo™ Therapy (Figure 1). This combination system allows instillation solutions to be delivered to the wound bed to help manage complex, difficult to-heal wounds, before converting to standard NPWT for further wound therapy. The V.A.C.Ulta™ System eliminates the need for a separate NPWT unit and manual application of a topical instillation solution between NPWT cycles (10).
A prospective study of patients with the diagnosis of complex, open, infected wounds that were treated with NPWT with instillation (0.5% silver nitrate solution) this group was compared to a retrospective control group of patients treated with standard moist wound-care therapy showed a significant reduction in average days of wound treatments, average days to clear infection, average days to wound closure and average days of hospitalization in the patients treated with NPWT with instillation (11).
Retrospective, historical cohort-controlled study to assess the effectiveness of Negative Pressure Wound Therapy (NPWT) versus Negative Pressure Wound Therapy with Instillation (NPWTi) in the treatment of infected wounds that require hospital admission and serial surgical debridement showed a significant reduction in number of operating room visits, time to final surgical procedure, length of hospital stay and percentage of wound closure in the patients treated with NPWT with instillation (13).
Prospective, randomized trial was to evaluate the effectiveness of NPWTi-d on biofilm of chronic wounds showed a significant reduction in quantitative biofilm-protected bacteria after one week of treatment (12).
Cases Presentation:
We present a case of a 24 years old, Indian male who admitted to the hospital on (1st of July 2019) after been bitten by an insect in a farm in India 10 days ago, there were no any signs and symptoms after bite, but 2 days ago patient started to have drainage, discharge bloody, streaking redness and black, hotness, pain (9/10) and erythema to Left lower extremity (Wound infection), The course/duration of symptoms is worsening as there were associated symptoms like fever and vomiting, patient was moderate distress, ill-appearing.
Patient clinically in general was alert and oriented to person, place, time, and situation, no focal neurological deficit observed, normal sensory observed, normal motor observed, normal speech observed, normal coordination observed.
Patient was diagnosed as Cellulitis, lymphangitis, skin ulcer, lymphadenitis, post-traumatic wound infection, necrotizing fasciitis.
3rd of July debridement was done for the left lower limb necrotizing fasciitis (Figure 2), as swelling was reaching before the procedure to upper thigh with area of necrotic skin lateral aspect edema and swelling down to the ankle and foot. Gauze applied after the procedure and the procedure tolerated very well and specimen sent to pathology and the following medications were started:
- Albumin Human 20% Injection (50 mL) 200 mL, IV, Daily
- Linezolid 600mg/300mL Injection 600 mg 300 mL, IV, q12hr
- Metoclopramide 10mg/2mL Injection 10 mg 2 mL, IV, q8hr
- Paracetamol 10 mg/mL (100 mL) Injection 1,000 mg 100 mL, IV, q6hr
- Piperacillin/ Tazobactam Sodium 4g/ 500mg Injection 4.5 gm 1 vial(s), IV, q8hr
- Dextrose 4.3% with 0.18% NaCl solution 2500 mL 2,500 mL, IV, 104.17 mL/hr
- Tramadol 100mg/2mL Injection (CD) 50 mg 1 mL, IM, q12hr
4th of July patient status was stable with no any general abnormalities but still there was swelling on the left leg with redness up to the thigh. Same antibiotics was continued, and patient transferred to the floor. Many debridement and dressing changes were done, and patient was stable but with no prognosis for the wound.

11th of July debridement was done and wound washed with Dermacyn then NPWTi was applied (NPWTi unit, Foam dressing, Container, Solution delivery kit) and setting were as following (125 mmHg negative pressure, 6 hours NPWT interval, 20 minutes dwelling time and 140 ml of Dermacyn) Figure (3).
16th of July dressing was changed with obvious granulation tissue formation and blood was transfused as patent’s HP was less than 12 as we need to elevate HP which accelerate healing of the wound Figure (4).


22nd of July NPWTi was applied again on the same setting (125 mmHg negative pressure, 6 hours NPWT interval, 20 minutes dwelling time and 140 ml of Dermacyn).
24th of July patient was started with alternate day dressing (Caciplique & Aquacel).
29th of July skin graft was done for the lower lift limb wound and patient suffered of hypotension during surgery which managed with administration of intravenous normal saline and one unit of blood Figure (5).
1st of August dressing was changed on the graft and was looking clean but right thigh dressing was opened and soaked with blood.
5th of August dressing changed and graft was very well with some blood oozing.
19th of August wound on the lift lower limb was re- grafted with split thickness skin meshed graft after been debrided under general anesthesia, then fixed with staples. The graft covered with Jelonet & diluted betadine gauze and donner site on both thighs covered with Nanoskin & pressure bandage. As estimated procedure blood loss was 300 ml. Offloading was applied as there was pressure injury on the left heel.
22nd of August dressing was changed over the graft and dressing over donner site was kept as it is without changing as there was no complication (Wet dressing & smell).
25th of August graft was taken except small area on the anterior aspect of the upper leg there was purulent discharge and dressing over donner removed as well with no complications Figure (6). Caciplique application on the donner wounds and raw areas on the left leg, Aquacel application on both thighs and daily dressing (With petadine) for left leg grafted wounds and physiotherapy was ordered for left lower limb. Patent wounds totally healed, and patient was discharged on 8th of September.


Discussion:
This case illustrated a significant effect of NPWT with instillation in cleaning up of the wound and reduction of pathogen bioburden, preparation of the wound bed as it accelerated the healing process and granulation tissue formation for the next step which was grafting of the wound and shortcut the total needed healing time.
References:
- “Necrotizing Fasciitis: A Rare Disease, Especially for the Healthy”. CDC. June 15, 2016. Archived from the original on 9 August 2016. Retrieved 13 August 2016.
- Bilton B, Zibari G, McMillan R, Aultman D, Dunn G, McDonald J. Aggressive surgical management of necrotizing fasciitis serves to decrease mortality: a retrospective study. Am Surg. 1998;64:397-400; discussion 400-1.
- Fleischmann, W., Russ, M., Westhauser, A., Stampehl, M. [Vacuum sealing as carrier system for controlled local drug administration in wound infection]. Unfallchirurg 1998;101:649-654.
- Gabriel A, et al.(2008), Negative pressure wound therapy with instillation: a pilot study describing a new method for treating infected wounds, Int Wound J; 5(3):399-413.
- Hakkarainen, Timo W.; Kopari, Nicole M.; Pham, Tam N.; Evans, Heather L. (2014). “Necrotizing soft tissue infections: Review and current concepts in treatment, systems of care, and outcomes”. Current Problems in Surgery. 51 (8): 344–62. doi:10.1067/j.cpsurg.2014.06.001. PMC 4199388. PMID 25069713.
- https://academic.oup.com/cid/article/44/5/705/348724
- https://www.healthline.com/health/necrotizing-soft-tissue-infection
- Kim PJ, et al.,(2014), The Impact of Negative-Pressure Wound Therapy with Instillation Compared with Standard Negative-Pressure Wound Therapy: A Retrospective, Historical, Cohort, Controlled Study, Plast Reconstr Surg; 133(3):709-16.
- Negative Pressure Wound Therapy with Instillation:Consensus Guidelines.
- Paz Maya, S; Dualde Beltrán, D; Lemercier, P; Leiva-Salinas, C (May 2014). “Necrotizing fasciitis: an urgent diagnosis”. Skeletal Radiology. 43 (5): 577–89. doi:10.1007/s00256-013-1813-2. PMID 24469151.
- V.A.C.Ulta™ NPWT System, Made Easy, Volume 3 | Issue 3 | September 2012,www.woundsinternational.com.
- Wilson, B (1952). “Necrotizing fasciitis”. The American Surgeon. 18 (4): 416–31. PMID 14915014.
- Yang C, Goss SG, Alcantara S, Schultz G, Lantis JC, (2017), Effect of Negative Pressure Wound Therapy With Instillation on Bioburden in Chronically Infected Wounds, Wounds.