Case Study
Introduction: Negative pressure wound therapy (NPWT) has been shown to be effective in the treatment of dehisced surgical wounds. This case study presents a patient whom had NPWT with instillation and the positive results it had in wound healing.
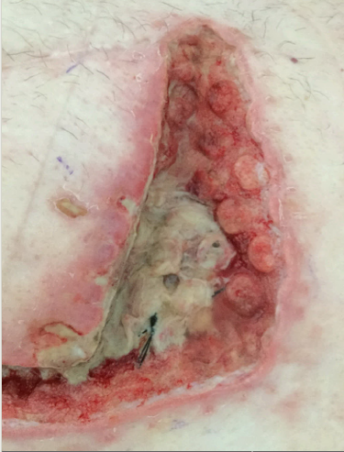
Patient Profile: A 65 year old gentleman had an elective hepatojejunostomy. The risks factors for this gentleman were that he had an autoimmune disease which he took long term steroids for and was overweight. His initial recovery from surgery was complicated as he developed a hospital acquired pneumonia which required him to be transferred to a high dependency unit for 4 days. Following this he was discharged from hospital on day 9 post-operative. He was readmitted on day 10 as he developed a wound infection (Photo 1).

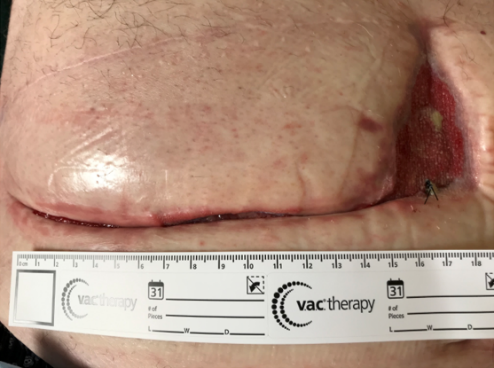
The wound was initially treated with standard VAC therapy. Following the first dressing change (Photo 2 and 3) it was decided that the complexity of the wound prevented the patient from being discharged from the hospital, as it was considered too large to be managed in the community. It was decided to commence VAC Vera Flo therapy with Cleanse Choice dressing.


Application of Therapy: Veraflo Cleanse choice dressing was applied on day 15 post op. This was instilling normal saline (NACL) 0.9% every 4 hours, with negative pressure at 125mmgh. The wound is a reverse L shaped would with the following wound measurements:
- 2.5 cm in the thinnest section of the vertical incision
- 4.5 cm wife in on the widest section of the vertical incision
- Length of vertical incision 10cm
- Tunneling was 1.5 cm
- Length of transverse section 13 cm
The patient had now been placed on targeted oral antibiotics following a positive wound swab culture.
Progress: After 2 days of Veraflo therapy, there was a noticeable improvement in the wound (Photo 4 and 5). There was a reduction in sloughy tissue on the wound bed and columns of granulation tissue had formed. The erythema that was previously surrounded the wound had almost completely resolved. The patient reported a noticeable difference in the wound, which provided reassurance to him that the wound was healing. The NACL solution was now being instilled on a 3 hourly cycle and negative pressure continued at 125 mmgh.
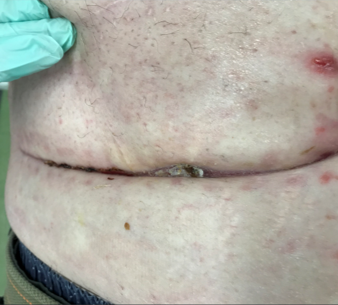
After 9 days of Veraflo therapy (Photo 6 and 7) there continues to be a decrease in sloughy tissue. The instillation of NACL assisted in cleansing the wound, softening this sloughy tissue and continuing to promote the formation of granulation tissue. The Veraflo therapy was continued for a total of 14 days (Photo 8 and 9).





Results: Veraflo therapy was seen to give results in days, with the instillation of NACL solution to soften the sloughy tissue on the wound bed, the holes in the cleanse choice dressing aiding the debridement of this tissue, working quickly to clean this infected wound. The patient did have to remain as inpatient to have the Veraflo therapy as the community nursing team did not have the skills to provide this wound treatment but if Veraflo therapy had not been commenced, it would be suggested that the patient would have had to remain in the acute care setting for longer while on standard VAC therapy due to the size of the wound. After 9 days of therapy the wound was now a size which was manageable for the community nursing team to provide appropriate wound care and the patient was discharged home with standard VAC therapy. Standard VAC therapy was continued for a further 35 days (Photo 10). Then the patient’s wound was dressed twice weekly with the dressing still being done on the date of case study mission (Photo 11 and Photo 12).

Conclusion and Recommendations:
This case study is an example of the appropriate use of VAC Veraflo cleanse choice therapy for treatment of a dehisced infected surgical wound. It has shown how negative pressure therapy with the addition of instillation of solution over the wound bed, can be effective in the treatment of complex wounds. Following on from this case study, it would be suggested for further education and training to be provided to both acute and community care nurses in Veraflo care to allow more patients to have access to this therapy and reduce the amount of time needed to spend in the acute care setting.