Case Study
Introduction
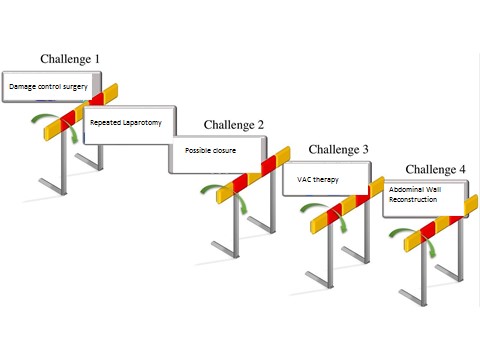
Management of an open abdomen continues to pose a challenge for surgeons. Multiple techniques for temporary abdominal closure have been described in the literature. Negative pressure wound therapy (NPWT) and synthetic or biologic repair materials are important tools in the management of open abdomen (1,2). It is essential that general and trauma surgeons understand the core principles underlying the need for and management of the open abdomen.
We report a case of a complex abdominal wound in a critically ill patient who underwent multiple laparotomies followed by abdominal wall reconstruction. NPWT was used initially and then replaced by V.A.C. VERAFLO™ Therapy. The frequent irrigation and suction reduced the chance of growth of bacteria and led to a significant reduction in bioburden. NPWTi is a valuable tool in the management of infected laparotomy wounds for open abdomen after damage control surgery.
Case Study: Application of negative pressure wound therapy with instillation (NPWTi) for complicated wound following abdominal wall reconstruction for an open abdomen.
Surgical procedures:
- Laparoscopic Sleeve gastrectomy (03/06/2014)
- Laparoscopic Revisional Roux-en-Y Gastric Bypass (LRYGB), for weight regain and reflux symptoms after Sleeve Gastrectomy (25/03/2019)
- Endoscopic control of bleeding after LRYGB (26/03/2019)
- Laparotomy, peritoneal lavage and repair of perforation at the jejuno-jejunal anastomosis (27/03/2019)
- Abdominal wall reconstruction, component separation, repair with BIO-A Reinforcement mesh and NPWT (07/04/2019).
- Replacement of NPWT by NPWTi to reduce the wound bioburden.
CASE DESCRIPTION:
Patient: 49-year-old male had laparoscopic revisional roux en-Y gastric bypass (RYGB) to change sleeve to RYGB on 25/3/2019 for post sleeve gastrectomy GERD symptoms. BMI was 33.
On a postoperative day one, the patient developed bleed from the first anastomosis which was seen clearly on endoscopy and clipped. Following the endoscopy, the patient became increasingly unstable and within 6 hours, the patient was required to go back to the operating room for laparotomy. He had jejuno-jejunal anastomotic perforation. Drainage, wash out and closure of perforated anastomosis was done. The abdomen was left open and Bogota’s bag was applied.
Despite complete closure of the peroration and abdominal washout and drains, he continued to deteriorate. On postoperative day three (on 27/3/2019), he was taken back for a second look laparotomy and found the entire repair intact and no secondary source in the abdomen. There was no abscess or infected fluid. The abdominal washout was done in all four quadrants as well as pelvis. There was no evidence of bowel obstruction and the abdomen was left open. He continued to remain in profound cardiovascular shock requiring high dose inotropic support and intensive care resulting in ECMO and CWHD therapy in the MICU where he was critical but improving. He also suffered from oliguric AKI-most likely ATN, bilateral LL DVT, ARDS and DIC as part of organ dysfunction due to septic shock.
On 07/04/2019 Midline laparotomy closure was done via component separation (anterior rectus sheath), BIO-A Reinforcement mesh 20 x 30 cm was applied.
Wound Management:
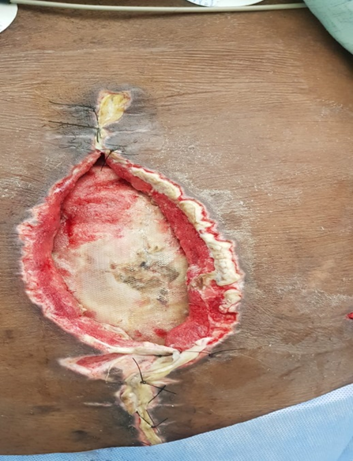
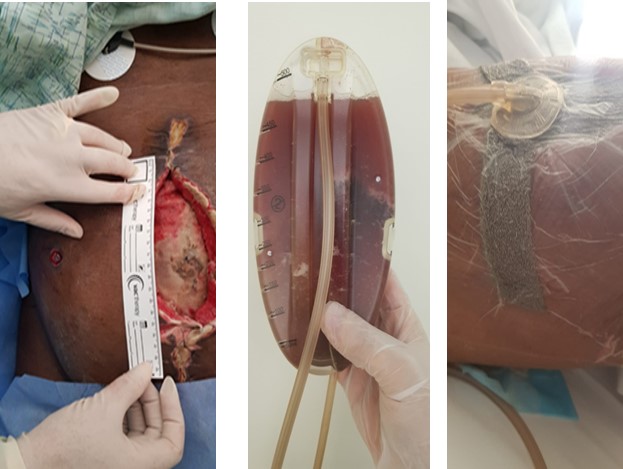
The patient was treated with different types of adjunctive wound therapy including NPWT. He was referred to the wound care team to assess the wound. It showed thick undermined edges, purulent fluid, bleeding fragile granulation tissue under the mesh and yellowish slough tissue at the upper & lower wound edges & the center of the wound. Drain sites were infected bilaterally with heavy thick discharge. The wound measured 27cm in horizontal diameter and 19 cm in vertical diameter and 2 cm in depth.
0n 15-4-2019, VERAFLO therapy (NPWTi) was applied to treat this wound as wounds treated with NPWTi had a significant reduction in bioburden compared to wounds treated with NPWT alone (3). NPWTi (VERAFLO therapy) applied with a medium pressure of 75 mmHg, instillation volume of 20 ml, soak time of 10 min every 4 hours, dressing changes every 2 days and canister change when full. Fluid irrigation helped to clear the infected fluids, debris and hemostatic powder used to control the bleeding. Application of NPWTi led to progressive wound healing, healthy granulation tissue, infection eradication, and enhanced wound bed preparation. The patient gradually improved and there was no complication related to the use of NPWTi such as bleeding or worsening local infection. NPWTi was used for 3 weeks with dressing changes every 2 days in the first week then every 3 -4 days in the 2nd and 3rd weeks. The frequent irrigation and suction reduced the chance of growth of bacteria and the requirement for wound bed debridement. After 3 weeks NPWT without instillation was used for 1 week. The patient was discharged home after complete wound healing.





Discussion:
The open abdomen is a relatively new and increasingly common strategy for the management of abdominal emergencies in both trauma and general surgery. The open abdomen can reduce mortality associated with conditions such as abdominal compartment syndrome, bowel perforation and internal organ laceration. Damage control surgery aims for first controlling immediate life-threatening events and then following with a later reparative surgery once the patient has stabilized to improve patient survival (4). However, the resulting open abdomen is a complex clinical problem (5,6). Patients who need an open abdomen experience a higher incidence of overall complications, including SIRS, MODS, fistulas, post-operative ileus, and third space fluid losses (6). Our patient had a complex clinical course. He developed refractory septic shock and severe respiratory failure that required ICU admission, respiratory, cardiovascular, renal support and ECMO. The abdomen was kept open and Bogotá bag was applied as a part of damage control surgery. Recent studies indicate both an improved survival rate and increased likelihood to successfully close a large proportion of patients, treated with open abdomen technique. Moreover, these patients can now be closed within the initial hospitalization (7).
Temporary abdominal closure techniques, such as the Bogotá bag or vacuum pack, have been described, along with other closure techniques, allowing the wound to granulate. The use of biodegradable mesh and sequential closure using NPWT allows surgeons to close most open abdomens. The Bogotá bag has been used in practice for more than 20 years. Despite the disadvantages, Bogotá bag has gained wide acceptance, and this technique was a starting point for the development of new devices for the prevention and treatment of abdominal compartment syndrome (ACS) (8). Bogotá bag was applied over the bowel after the first laparotomy for our patient and was replaced by NPWT in the second surgery.
The V.A.C. Therapy allows for rapid closure of the abdominal wall with application of continuous suction to control abdominal secretions. This technique applies subatmospheric pressure to the open abdomen through a reticulated polyurethane foam dressing. The device, dressings, tubing, and canisters are used as a complete system for negative pressure wound therapy. V.A.C. therapy will also help promote granulation tissue formation at the wound edges due to the contact of the foam with the wound margins and will help approximate wound edges to allow closure of the fascia and abdominal wall. Precaution should be taken when using V.A.C. therapy for patients with active bleeding, and V.A.C. dressings should not be placed over exposed blood vessels or organs.
NPWTi combines traditional NPWT with application of topical irrigation solutions within the bed of the wound. The mechanism of action allows for the delivery of instilled fluid to the wound bed facilitating a removal of cellular debris, exudate and other infectious material that may impair wound healing. Moreover, NPWTi decreases the bacterial bioburden within the wound and reduces biofilm formation. Fewer operative visits are required when using NPWTi compared to standard NPWT. Mechanical debridement, reduction of biofilm and autolytic mechanisms are considered the most important components of NPWTi action and they are key elements emphasizing the advantage of NPWTi over the standard NPWT (9). A study in Mexico assessed NPWT with instillation in abdominal wall reconstruction cases relative to conventional treatment and found that there was an increased rate of fascial closure, shorter intensive care unit (ICU) stay, and decreased mortality (10).
After abdominal reconstruction with component separation, the wound showed purulent discharge, debris and thick adherent blood clots under the mesh. V.A.C. VERAFLO™ Therapy was used to clear the thick fluids and dissolve the hemostatic powder that was used to control bleeding during surgery. The drain output was brownish purulent initially and slowly became serosanguinous and later became clear. After 3 weeks of V.A.C. VERAFLO™ Therapy, traditional NPWT was resumed. The wound showed great improvement, marked reduction of wound size followed by complete wound healing and the patient was discharged home safely.
Economic value:
The usage of NPWTI reduced the frequency of dressing changes, in turn, reduced the nursing time for dressing changes. The therapy also reduced the chance of growth of bioburden bacteria by frequent irrigation and continuous pressure mode, and in-addition reduced the wound bed debridement incidence.
Conclusions:
This case report demonstrates the successful use of the NPWT with instillation system to aid in complete secondary intention healing of a large abdominal wall defect following damage control laparotomy and abdominal wall reconstruction. NPWTiproved to be a valuable tool in the management of infected laparotomy wounds for open abdomen after damage control surgery. Future studies and continued innovation will hopefully lead to better understanding of optimal treatment strategies for these devastating injuries.
References:
- Perathoner A, Margreiter R, Kafka-Ritsch R: Surgical treatment of the open abdomen in patients with abdominal sepsis using the vacuum assisted closure system. World J Surg. 2009;33(6):1332–1333. Author reply 1334.
- Sharrock AE, Barker T, Yuen HM, Rickard R, Tai N: Management and closure of the open abdomen after damage control laparotomy for trauma. A systematic review and meta-analysis. Injury. 20
- Goss SG, Schwartz JA, Facchin F, et al. J Am Coll Clin Wound Spec. Vol. 4. Spec: 2014. Negative pressure wound therapy with instillation (NPWTi) better reduces post debridement bioburden in chronically infected lower extremity wounds than NPWT alone; pp. 74–80. [PMC free article] [PubMed] [Google Scholar]
- Supplement to wounds: a compendium of clinical research and practice; October 2005 (p. 1 – 22) Nicholas JM, Rix EP, Easley KA, et al. Changing patterns in the management of penetrating abdominal trauma: the more things change, the more they stay the same. J Trauma. 2003;55(6):1095–1110.
- Johnston M, Safcsak K, Cheatham ML, Smith CP: Management of the open abdomen in obese trauma patients. Am Surg. 2015;81(11): 1134–1137.
- Open Abdomen Advisory P, Campbell A, Chang M, et al: Management of the open abdomen: from initial operation to definitive closure. Am Surg. 2009;75(11 uppl):S1–S22.
- Boele van Hensbroek P, Wind J, Dijkgraaf MG, Busch OR, Goslings JC: Temporary closure of the open abdomen: a systematic review on delayed primary fascial closure in patients with an open abdomen. World J Surg. 2009;33(2):199–207.
- Ferrada R, Birolini D. New concepts in the management of patients with penetrating abdominal wounds. Surg Clin North Am. 1999;79(6):1331–1356.
- A. Gabriel, J. Shores, C. Heinrich, W. Baqai, S. Kalina, N. Sogioka, and S. Gupta, “Negative pressure wound therapy with instillation: a pilot study describing a new method for treating infected wounds,” Int Wound Journal, vol. 5, no. 3, pp. 399–413, jun 2008.
- Sibaja P, Sanchez A, Villegas G, Apestegui A, Mora E: Management of the open abdomen using negative pressure wound therapy with instillation in severe abdominal sepsis: a review of 48 cases in Hospital Mexico, Costa Rica. Int J Surg Case Rep. 2017, 30:26-30.
Excellent study showing the value of VAC VERAFLOW Therapy
Excellent study indicating the value of VAC VERAFLOW Therapy
A very detailed study show the efficacy of veraflow therapy for the patients .
excellent
it was very challenging case as many co-morbidities such as septic shock were presented and the outcomes are credible and outstanding.