Case Study
Introduction:
Global incidence of diabetes has imminently increased in the last 30 years, with nearly 422 million adults
worldwide now diagnosed with the disease, increasing global prevalence from 4.7% to 8.5%
(WHO, 2016). Within the diabetic population, the incidence of DFUs has been reported to
be between 4% and 10%, with a one-in-four risk of developing a DFU over a patient’s lifetime
(WUWHS, 2016; Armstrong et al, 2017).
Around 50% of DFUs become infected, and in approximately 20% of these patients, infection will
lead to amputation (Wu et al, 2007).
One of the most emerging therapies in past 20 years is treating diabetic wounds with V.A.C.® Therapy; which can result in faster wound bed preparation, a faster closure, and in a better graft take rate when compared to standard wound care. (Dalla Paola L, et al.
2010)
NPWT w/instillation was introduced first time in 1998 (Lehner et. al, 2011). It was suggested that using NPWT w/instillation after proper debridement, was sufficient to shift the wound healing trajectory from risk of infection and delayed healing to granulation formation. (Brinkert D, et al 2013)
There are a number of additional factors to consider when NPWT is used in the presence of
infection, including (Wounds Middle East 2016):
- Debridement or removal of devitalized tissue
- Appropriate antibiotic therapy
- Frequent assessment of the patient and wound
- Increased frequency of dressing changes
- Appropriate pressure settings on the NPWT system
- Peri wound skin protection
- Use of fenestrated antimicrobial dressings.
DFU Assessment:
Thorough holistic assessment approach is recommended utilizing MDT (Multi-disciplinary team) approach, taking into consideration the following parameters:
Initial assessment should include evaluation of (WUWHS, 2016):
-
- Diabetes management and blood glucose control
- Previous history of foot ulceration and surgery
- Smoking status
- Symptoms and signs of peripheral arterial or venous disease
- Symptoms and signs of peripheral neuropathy
- Musculoskeletal evaluation, e.g. for overall flexibility, range of movement in the ankle, foot shape
- Systemic signs of infection
- Pain, e.g. neuropathic pain, wound-related pain
- Socioeconomic circumstances, dexterity, visual acuity and insight.
Management protocols:
- Offloading should be considered a key first-line treatment in suitable patients. If a person
with diabetes has a lesion on the sole of their foot, offloading body weight is of vital importance; all therapeutic efforts are bound to fail if he or she continues to walk on an ulcer (Shankhdhar et al, 2009).
- Regular debridement is an important aspect of DFU management and aims to remove slough,
non-viable tissue and hyperkeratotic wound margins (callus). Sharp debridement carried out by experienced clinicians with specialist training is widely used in treatment of DFUs but should be used with caution in a patient with an ischaemic foot (WUWHS, 2016).
- In deep/cavity wounds where infection is present, negative pressure wound therapy (NPWT) or NPWT with instillation may be considered. NPWT with instillation can be used with saline or antimicrobial agents that have been assessed for device compatibility to reduce the potential for wound infection (Wounds International 2017)
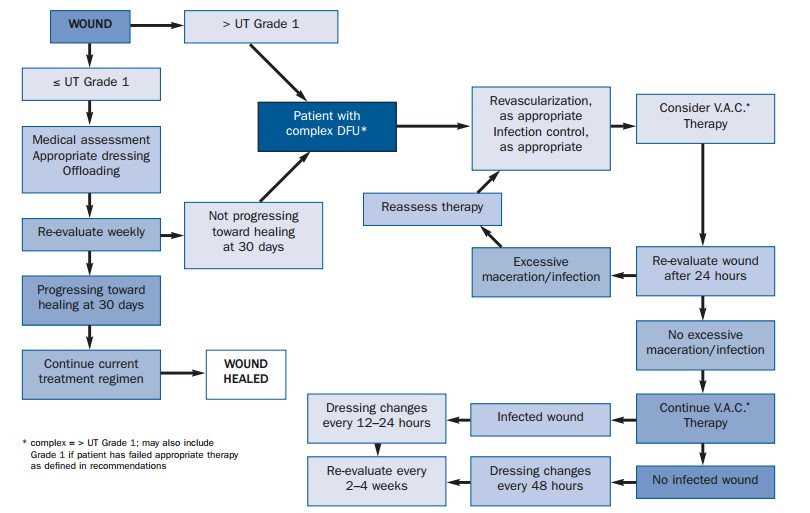
- Below are some recommended algorithms to manage DFUs based on classification, Adapted from Andros et al (2006) Consensus statement on NPWT for the management of diabetic foot wound: (Figure A):
Case report:
Patient details: A 64 years old male patient, known case of Diabetes Mellitus who was admitted as a case of left Diabetic foot. Admitted on 2nd of June 2019.
Initial assessment: left foot diabetic foot ulcer (Heel to Planter to Lateral and medial to lateral side) (Figure C)
Debridement performed twice: 3rd of June and 12th of June. (Figure D)
Wound assessment on 17th of June: 20% Granulation, 20% Dry Slough, and 60% Necrotic tissue.
Probed to Calcaneal bone.
Moderate to Purulent discharge
Erythema in the peri-wound, foot swelling
Multiple tunneling in different area of the wound
Procedure: Wash with Betadine, Dermacyn (Super-Oxidized water) solution, and Chlorohexidine wash.
Ultra-sonic debridement done.
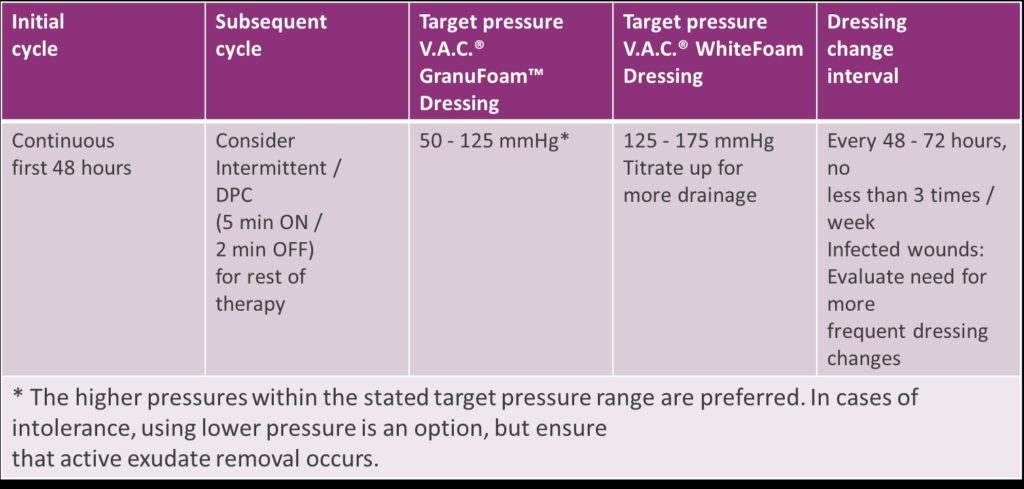
Initiate NPWT w/instillation (20 ml Dermacyn (Super-Oxidized water), 3 mins soak time, and 3 hours VAC cycle on -125 mmHg) using VeraFlo dressing by KCI company – USA.
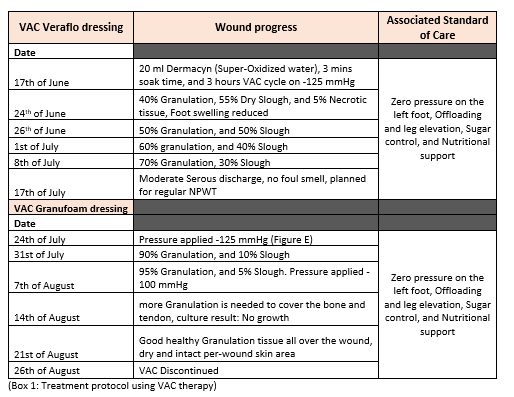
Grafting: 3rd of Sept. patient had a split-thickness skin graft from the medial aspect of the Thigh, covered with Inadine dressing and protected by Mepilex Ag as a secondary dressing(Figure F).
Patient follow up: patient came back 4 weeks post-op for follow up, graft has taken in almost 80% of wound surface area (Figure G).





Summary:
The use of negative pressure in conjunction with instillation provides an important evolution
in the negative-pressure wound therapy concept with the potential added benefit of supplying an
antimicrobial solution to the wound bed. (Kim et al. 2013). NPWT w/instillation can be used to treat Diabetic wounds as per 100% consensus agreement (Kim et. Al 2013).
Some studies indicated that use of NPWT can minimize the rate of lower extremity amputation in diabetic patients Vs. use of Moist Wound healing dressing. (Frykberg and Williams, 2007; Bernstein BH, et. al, 2005). It is empirical to understand the challenges remain with regards to accurate diagnosis, and effective and appropriate treatment, of wound infection. Yet, there is a need to focus on building a strong evidence base for use of NPWT w/instillation as an advanced treatment for complex wounds and as an adjunct for prevention and management of infection. Therefore, it would be of significance to document success and failures using such modality on different complex DFUs and share experiences, and to collect data from RCTs to help build the evidence base.
References:
- Andros, G., Armstrong, D.G., Attinger, C.E., Boulton, A.J., Frykberg, R.G., Joseph, W.S., Lavery, L.A., Morbach, S., Niezgoda, J.A. and Toursarkissian, B., 2006. Consensus statement on negative pressure wound therapy (VAC® Therapy) for the management of diabetic foot wounds. Wounds, 18(6).
- Armstrong D, Boulton AJM, Bus SA (2017) Diabetic foot ulcers and their recurrence. New Eng J Med 376: 2367-75
- Banwell, P., 2007. VAC® Therapy Clinical Guidelines. London. KCI Europe Holding.
- Bernstein, B.H. and Tam, H., 2005. Combination of subatmospheric pressure dressing and gravity feed antibiotic instillation in the treatment of post-surgical diabetic foot wounds: a case series. Wounds, 17(2), pp.37-48.
- Brinkert, D., Ali, M., Naud, M., Maire, N., Trial, C. and Teot, L., 2013. Negative pressure wound therapy with saline instillation: 131 patient case series. International wound journal, 10(s1), pp.56-60.
- Dalla Paola, L., Carone, A., Ricci, S., Russo, A., Ceccacci, T. and Ninkovic, S., 2010. Use of vacuum assisted closure therapy in the treatment of diabetic foot wounds. J Diabetic Foot Complications, 2(2), pp.33-44.
developing world. Diabetes Voice 54(3): 27-9
- Frykberg, R.G. and Williams, D.V., 2007. Negative-pressure wound therapy and diabetic foot amputations: a retrospective study of payer claims data. Journal of the American Podiatric Medical Association, 97(5), pp.351-359.
- Identification and management of infection in diabetic foot ulcers, international consensus roundtable meeting 2017, available at https://www.woundsinternational.com/resources/details/identification-and-management-infection-diabetic-foot-ulcers (accessed 13.10.2019)
- Kim, P.J., Attinger, C.E., Steinberg, J.S., Evans, K.K., Lehner, B., Willy, C., Lavery, L., Wolvos, T., Orgill, D., Ennis, W. and Lantis, J., 2013. Negative-pressure wound therapy with instillation: international consensus guidelines. Plastic and reconstructive surgery, 132(6), pp.1569-1579.
- Lehner, B., Fleischmann, W., Becker, R., & Jukema, G. N. (2011). First experiences with negative pressure wound therapy and instillation in the treatment of infected orthopaedic implants: a clinical observational study. International orthopaedics, 35(9), 1415–1420. doi:10.1007/s00264-011-1274-y
- Shankhdhar LK, Shankhdhar K, Shankhdhar U, Shankhdhar S (2009) Offloading the diabetic foot in the
- World Union of Wound Healing Societies (2016) Position document: Management of biofilm. Available at: http://www.woundsinternational.com/wuwhs/view/position-document-management-of-biofilm (accessed 30.09.2019)
- World Union of Wound Healing Societies. Position document: Local management of diabetic foot ulcers, 2016. Available at: http://www.woundsinternational.com/wuwhs/view/position-documentlocal-management-of-diabetic-foot-ulcers (accessed 28.09.2019)
- Wound healing and infection Evidence-based recommendations for NPWT in the prevention or management of infection Using NPWT with instillation in practice 2016, available at https://www.woundsme.com/resources/details/wounds-international-middle-east-expert-forum-npwt-infected-wounds (accessed 13.10.2019)
- Wu S, Driver VR, Wrobel JS et al. Foot ulcers in the diabetic patient, prevention and treatment. Vasc Health Risk Manag 2007; 3(1): 65-76