Case Study
- Introduction
In our Department of Visceral Surgery, we provide medical care to a broad range of disease patterns One of the most challenging aspect in the clinical routine is the treatment of large-scale (extended) wounds. In order to avoid complications, as well as to reduce extended hospital stay, would healing disorder requires specific handling.
Mr. O.K is a 51 -year old white male who has been referred to the department for evaluation and treatment of pre-sternal abscess. His past medical history includes anxiety disorder and cancer phobia. We conducted an abscess excision. The histopathological investigation of the removed tissue assessed a R1 situation of an invasive Basalioma. A second resection was performed with the appropriate safety margin, followed by the histopathological R0 confirmation.
The wound dimension after the second operation was 10×12 cm² with a depth of 2 cm, partially reaching the pectoral muscle and sternum bone. Due to the pre-sternal localization, a secondary seam without considerable cosmetic impairment could not be performed.
The initial wound therapy with absorbent compress showed no granulation and the exudate rate increased. VERAFLO instillation protocol and therapy was explained and cleared with Mr O.K; Patient approved photo documentation for scientific purposes.
- Methods
- Wound debridement under general anesthesia
On 9.8.2019, we performed the surgical wound debridement under general anesthesia. Necrotic fat tissue were removed.
- VERAFLO instillation therapy
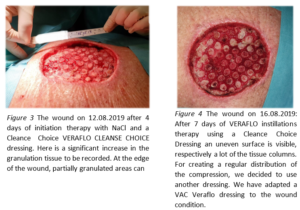
VERAFLO therapy started on 09.08.2019 with a suitable, adjusted VERAFLO CLEANSE CHOICE foam, completely filling the wound up to the skin level. The foil cover foam together with the allocated draig pad were connected to the Ulta KCI device. We used the following settings: instillation volume of 60 ml NaCl with an exposure time of 5 minutes followed by 3.5 hours of vacuum suction with a pressure of -125mm Hg.
- Vacuum dressing exchange
The vacuum dressing was changed every 4 days under sterile conditions in operating room.
- Nutritional plan
An individual nutritional plan was developed in order to achieve a balanced metabolism, avoiding large fluctuations between catabolic and anabolic conditions. For Mr. O.K. weighing 95 kg with 1.9 m body height (BMI 26.3 kg/m²), the necessary basal metabolism was 2280 kcal/24h, with an energy balance under wound healing condition of 3648 kcal/24h and a protein demand of 100g/24h. Based on patient meal preferences an individual nutrition plan was worked out.
- Prophylaxis of muscular atrophy
Only with a wound healing disorder and without any other organic disease the patient was able to perform a daily 60 min long motion program.
- Intraoperative surface anesthesia
A consistent, daily food intake and a motion program built a solid foundation for a balanced anabolic metabolism. To avoid a metabolic dis-balance due to the required fasting before a general anesthesia, we chose to conduct the Vacuum dressing excenge under local anesthesia. We used 20 ml Xylocain 5%. After turning the Ulta KCI device off and clamping the flexible tube, we injected the Xylocain into the foam and waited approx. 30 minutes for the drug to take full effect.
- Local analgesia during the suction phase
Mr. O.K. reported pain during suction phases. In order to reduce the risk of a sudden therapy withdrawal, the NaCl instillation solution was supplemented with Xylocain 5% (20 ml Xylocain 5% in 500 ml NaCl). After that the patient was also pain free during the suction phase, requiring no additional pain medication.
- Patient mobility
Mr. O.K. was pretty active and enjoyed his daily physiotherapy. The only disruption was the unpleasant feeling due to the glue foil on his chest and the weight of the device he needed to carry with him. By slicing the foil into 2 cm thin strings and gluing them accordingly to his skin fold directions, we were able to solve the unpleasant, foreign- body feeling the patient mentioned. To facilitate the walk with the needed the device, we made a walker with a basket available.

- Results
The first operation, an abscess excision, was performed on 1.8.2019. The second excision took place three days later on 4.8.2019. The wound was treated conservatively (without vacuum therapy) between 4.8.2019 and 9.8.2019. With the incoming of the final histology we begun with the VERAFLO instillation therapy (9.8.2019). The picture 1 shows that no granulation tissue is developing under conventional wound therapy. High exudate rates prohibit wound healing.



- Conclusions
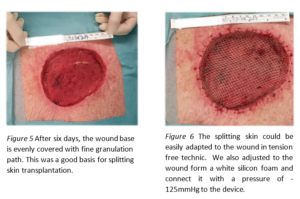
Through the VERAFLO instillation therapy, we had the opportunity to offer our patients an accelerated wound healing. In the size of the wound, the increased amount of exudate and due to the unfavorable position of the wound it would have taken a long time under conventionaly wound managemant to reach a good wound base, where one could perform a splitting skin transplant.
We have intensively cared for the patient. The close and prolonged monitoring made possible for us to observe many positive and negative aspects of VERAFLO instillations therapy and thus act accordingly.
Mr. O.K. recovered well and was discharged after 23 days. His discharge protocol included wound care and observation as needed, by our wound experts and weekly consultation to monitor his progress. Six weeks, post- op, patient has been cleared to return to work as a bus driver with no limitations.
Thanks to the VERAFLO instillation therapy and our intensive and extensive treatment, we were able to achieve a quick and exemplary wound healing
- Proposals
To ensure that the patient is not restricted in his mobility, a stable means of transport is necessary for the device. The Patients with wound healing disorder or with a large wound, the patients who need a VERAFLO instillation therapy are usually restricted and cannot carry the device around with them. My suggestion is to mount the device on a rollator.
Suggesting to rearrange order of paragraph as per below
The Patients with wound healing disorder or with a large wound, candidates for a VERAFLO instillation therapy are usually restricted and cannot carry the device around with them. To ensure that the patient is not restricted in his mobility, a stable means of transport is necessary for the device. Thus, I am recommending to mount the device on a rollator.
Patient data and images used with permission from PD Dr. Thilo Schwandner, Medical Director and Head of General and Visceral Surgery Departmnet, Asklepios Hospital Lich, Germany