Case Study

Introduction
A pressure ulcer is injury to the skin or underlying tissue due to the effects of pressure and or sheer (EPUAP, 2016). They can potentially occur in any individual, healthy or ill, young or old who sustains significant or sustained pressure and sheer forces. The prevalence of pressure ulcers in Ireland is 15%, ranging from 4% in the community to 37% in spinal cord units (Moore, No date).They are not simply another wound but hey have a significant impact on the emotional, psychological and physical wellbeing of patients (Moore and Cowman, 2009). In addition, there is an associated increased cost due to increased length of stay and care interventions (Bennett et al, 2004). In order to promote healing not only does the wound bed need to be optimized but the area needs to be off loaded. The following case study outlines the use of V.A.C. VeraFlo™ Dressing (KCI USA, Inc, San Antonio, TX) in healing a complex Category 4 pressure ulcer.
Case presentation
Mr M was a 59 year old gentleman who thirty years previous had sustained a traumatic T12 spinal cord injury that left him paraplegic. Mr M used a wheelchair, was independent with his activities of daily living and working full time. Initially he thought that he had developed an abscess on his buttock and that it would be self limiting. Over time the exudate increased and he attended his primary care team. There was an attempt made by the community to heal the wound using the Smith and Nephew Renasys negative pressure system. The wound became infected and he presented though the Emergency Department with signs of sepsis (tachycardia 110bpm, temperature 39oC, CRP 250mg/L, white blood cells 15.3×109/L, neutrophils 13.8×109/L, lymphocytes 0.8×109 /L) and cellulitis.
The wound was over his left ischialtuberositiy and thus was most likely a pressure ulcer. On admission to the hospital the opening of the wound was 7.8×5.5cm, however there was extensive undermining. There was a large amount of offensive smelling, thick green exudate. A wound swab showed the presence of Enterobacter and Escherichia coli. An MRI demonstrated the presence of osteomyelitis in the left ischium and pubic bone, over an
anteroposterior distance of 8.3 cm and a craniocaudal distance of 7.7 cm.He was started on Tazocin on admission but changed to Ciprofloxacin when the sensitivities became available and showed the E. coli was resistant to Tazocin. He received a review by the plastics team who felt a washout and debridement was needed.
Treatment with NPWTi
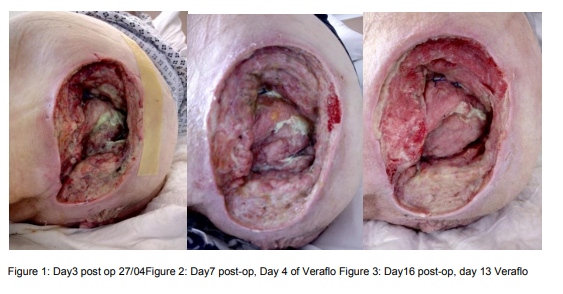
On Day 3 post wound debridement the post-operative dressing was removed, the wound measured 14.5×7.5x4cm (see figure 1), bone was visible. There continued to be large amounts of offensive smelling, thick green exudate. A decision was made with the Tissue Viability Nurse, Plastics consultant and Mr M, to use negative pressure wound therapy with instillation. This decision was made as the wound would benefit from the rapid granulation that occurs with negative pressure in addition to the cleansing that the instillation would offer.
Saline was chosen as the instillation solution.
The V.A.C. VeraFlo™ Dressing (KCI USA, Inc, San Antonio, TX) was changed every 48- 72hours. The wound was instilled with 100mls of saline for 10 minutes every 3 ½ hours, with continuous negative pressure at -125mmHg. Due to the proximity of the wound to the anus (approx 1cm) V.A.C. Gel strips were used to ensure a good seal. With the size of the wound, the wound exudate and the fluid for instillation, the intensity was set to high. The dressing was bridged up onto Mr M’s abdomen so that he would not be seated on the SensaTrac tubing.
Four days after VeraFlo was commenced the wound had improved dramatically (Figure 2). There was less purulent exudate, the odour had been eradicated and the wound was beginning to granulate.
Dressings continued to be changed as outlined previously. However, Mr M was an independent and mobile gentleman and VeraFlo therapy was impacting on his quality of life. The Ulta unit is large and heavy, Mr M was a wheelchair user and it restricted his mobility. In addition due to the fluid associated with the wound and the location, leaks occurred. These needed nurse intervention, disruption to Mr M’s day and intimate care.
On day 13 of Veraflo therapy (Day 16 post-op) the wound measured 13x10x3cm. The wound bed was granulating well and significantly less sloughy. The irregular nature of the wound and the hip flexion affected the accurate wound measurements. A decision was made in conjunction with Mr M to stop the VeraFlo therapy and switch to the V.A.C.® GranuFoam™ Dressing (KCI USA, Inc, San Antonio, TX), using the ActiV.A.C. unit.
The negative pressure therapy was again delivered at -125mmHg, continuous pressure at high intensity, with dressings changed every 48-72 hours. Twenty-two days post wound debridement Mr M was discharged. On day of discharge (day 22 post-op) the wound measured 12.5×7.5×2.5cm.The negative pressure wound therapy continued post discharge in the community.
Ten weeks post-op Mr M was readmitted into a tertiary hospital under the same plastic surgeon and had a flap reconstruction (Figure 4). Over one year on the wound remains closed with no further issues.

Discussion
Mr M was a large infected pressure ulcer, that post debridement had a large defect that needed substantial new tissue growth to close. The use of the Veraflo allowed continuous washout of the wound and prevented Mr M having to return to theatre. This reduced patient exposure to anesthetic, reduced theater time and associated staff and consumable costs; it allowed Mr M to carryout his activities of daily living without fasting or the effects of anesthetic. It is clear to see from Figures 1-3 the effects of only 13 days of Veraflo in removing slough and promoting granulation tissue. Furthermore, his length of stay was shorter than one would have expected if using only conventional dressings, only 22days post-op.
The current consensus is for saline as the first choice of instillation solution in NPWTi (Kim et al, 2019). There exists some debate over whether this holds true for infected wounds. While the wound had positive swab cultures, most of the infected tissue had been removed during surgery and concurrent intravenous antibiotics were being administered. Thus to avoid any cytotoxic effects from antiseptic solutions saline was chosen.
A drawback of the Veraflo system is the use of the Ulta unit. It is large and bulky and impacted upon Mr M’s independence. He needed assistance to transfer into his wheelchair and the unit when placed on the back of his wheelchair decreased the chairs stability. A small unit would be beneficial for mobile, active patients.
Conclusions
There is no doubt that the use of the Veraflo system allowed such an extensive, infected wound to be cleaned and granulated to such an extent it was closed within ten weeks of debridement. Using conventional dressings would have taken months, increased the length of stay, would likely have increased the risk of further infection and necessitated further surgeries for debridement or washout. The Veraflo system is a useful tool to have in the healing of infected pressure ulcers.
References
Bennett, G., Dealey, C. and Posnett, J. 2004. The cost of pressure ulcers in the UK. Age and Ageing, 33 (3) p230–235 European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel. 2016. Prevention and treatment of pressure ulcers: quick reference guide. Washington DC: National Pressure Ulcer Advisory Panel. Kim, P.J., Attinger, C.E., Constantine, T., Crist, B.D., Faust, E., Hirche, C.R. Lavery, L.A., Messina, V.J., Ohura, N., Punch, L.J., Wirth, G.A., Younis, I. and Téot, L. 2019. Negative pressure wound therapy with instillation: International consensus guidelines update. International Wound Journal, 1–13. Moore, Z. No date. Pressure Ulcers.Available from https://www.hse.ie/eng/about/who/qid/nationalsafetyprogrammes/pressureulcerszero/pressur e-ulcers-to-zero-prof-z-moore-dublin.pdf (Accessed 01/12/19). Moore, Z. and Cowman, S. 2009. Quality of life and pressure ulcers: a literature review. Wounds UK 5 (1) p58-65.