Case Study
Mr C was a 64-year-old gentleman admitted with an infected abscess to the right calf. He had a history of long-term intravenous drug use and had previous hospital admissions involving multiple surgical debridements of the same site following injection of drugs.
His past medical history included COPD, Hepatitis C, Chronic bilateral venous leg ulceration, smoker. Prior to admission, he lived with his wife and was independent in all activities of daily living.
An MRI scan showed a 7.5cm x 1.2cm x 11cm collection overlying the gastrocnemius muscle and reactive myositis. Mr. C was placed on intravenous antibiotics and reviewed by the vascular team who ruled out the presence of peripheral vascular disease following an arterial duplex scan.
During his admission the calf was surgically debrided on three occasions. Following the first surgical debridement an ACTIV.A.C.™, using V.A.C.® GRANUFOAM™ Dressing was applied in theatre and Mr. C was referred to the Tissue Viability Service for ongoing management of the wound.
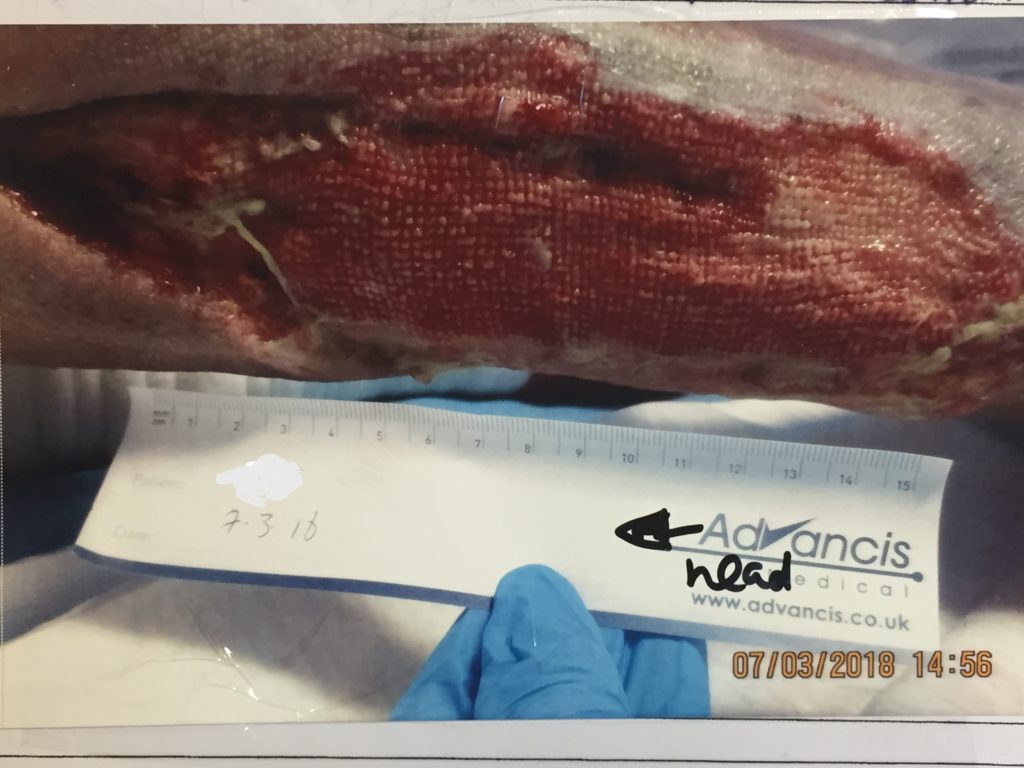
At the first assessment the Tissue Viability Nurse found the V.A.C.® GRANUFOAM™ Dressing was adhered to the wound bed and required soaking off which was both painful and distressing for the patient. Upon removal of the V.A.C.® GRANUFOAM™ Dressing, the wound measured 9.5cm x 7.5cm with undermining of 5cm in a proximal position. The wound bed had exposed tendon and necrotic tissue present. The wound edges were deep and rolled. Exudate levels were heavy and purulent. There was a strong malodour, indicating presence of infection.
Mr C had a further two surgical debridements which involved debriding 15cm achilles tendon followed by application of ACTIV.A.C.™ in theatre. Unfortunately the same problems occurred with rapid regrowth of slough and necrotic tissue.
At this stage Mr C was experiencing unrelenting pain to the lower leg which the ward staff were having difficulty managing. As a result he was referred the pain team for further assessment. He was unable to weight-bear and was propelling himself around the ward in a wheelchair.
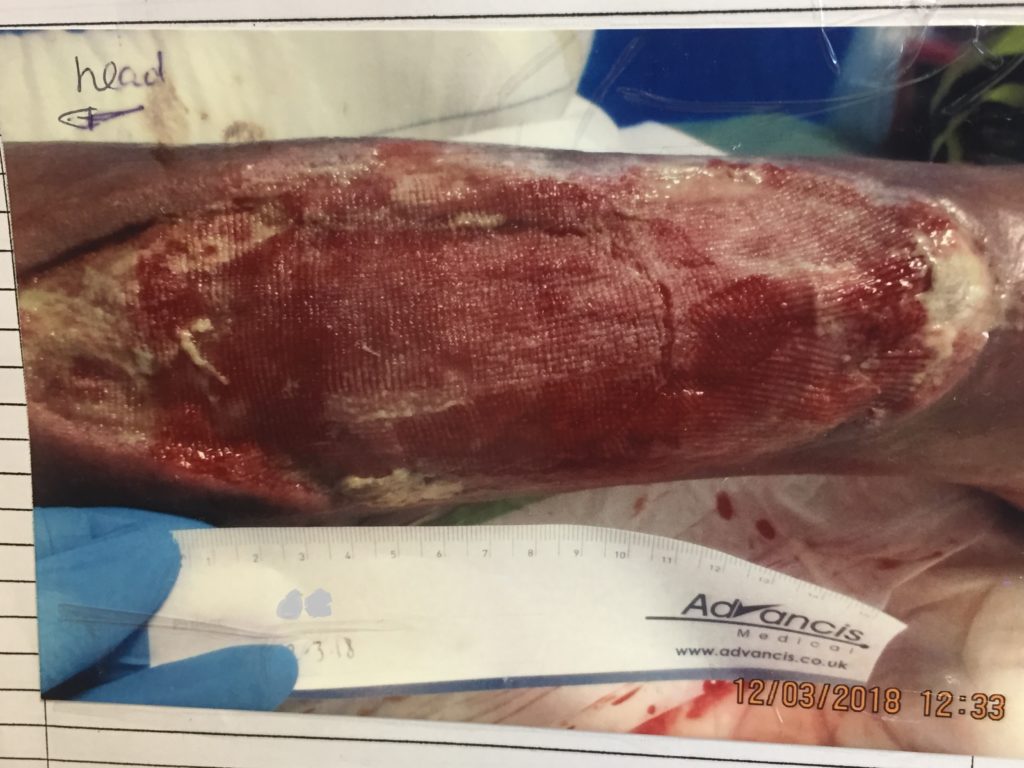
At this point the wound measured 20cm x 10cm and had a combination of exposed tendon, thick, wet slough, pus and granulation tissue and undermining of 4cm. As there was no improvement to the wound, the orthopedic team informed Mr C that they could not continue with ongoing debridements and were considering a below knee amputation. This was a distressing concept for him and his family and they stated that they wanted to avoid this action. It was then suggested to try V.A.C. VERAFLO™ Therapy to cleanse the wound with instillation of Prontosan® Wound Irrigation Solution (an irrigation solution containing PHMB ) to help control bacterial levels, which Mr C agreed to.
The surrounding skin was protected with Medi Derma-S – Medical Barrier Film and DuoDERM® Extra Thin. V.A.C. VERAFLO™ Cleanse Dressing, size large was applied to the wound which, due to its location and size required the patient to lie prone and two clinicians to apply the dressing. V.A.C. VERAFLO™ Therapy was initiated using volumetrically controlled Prontosan® Wound Irrigation Solution which was instilled until the foam was filled, with a 10 minute dwell time followed by 3.5 hours of continuous negative pressure at -125mmHg. The ward nurses were shown how to change the Prontosan® bottle once it was empty and action to take if the V.A.C. VERAFLO™ Unit began alarming.
Two days later
The V.A.C. VERAFLO™ Dressing was removed and the wound was visibly shallower at the distal aspect with an increase in granulation tissue and reduction of slough and necrotic tissue. Mr C had found the therapy comfortable and his pain levels were noticeably lower. Due to its hydrophobic properties, the V.A.C. VERAFLO™ foam does not usually require for the wound to be lined with non-adherent dressing. However, in the case of Mr C the foam did adhere to the wound bed and needed to be soaked off slowly which caused light trauma to the wound upon removal and pain to the patient.
The V.A.C. VERAFLO™ Dressing was reapplied but, Silflex, a soft silcone wound contact layer was used to line the wound (with exception to sloughy tissue to optimise cleansing / desloughing to area) prior to application of the foam. This proved to be successful in avoiding further adherence of the foam to the wound bed thus reducing trauma and pain upon removal.
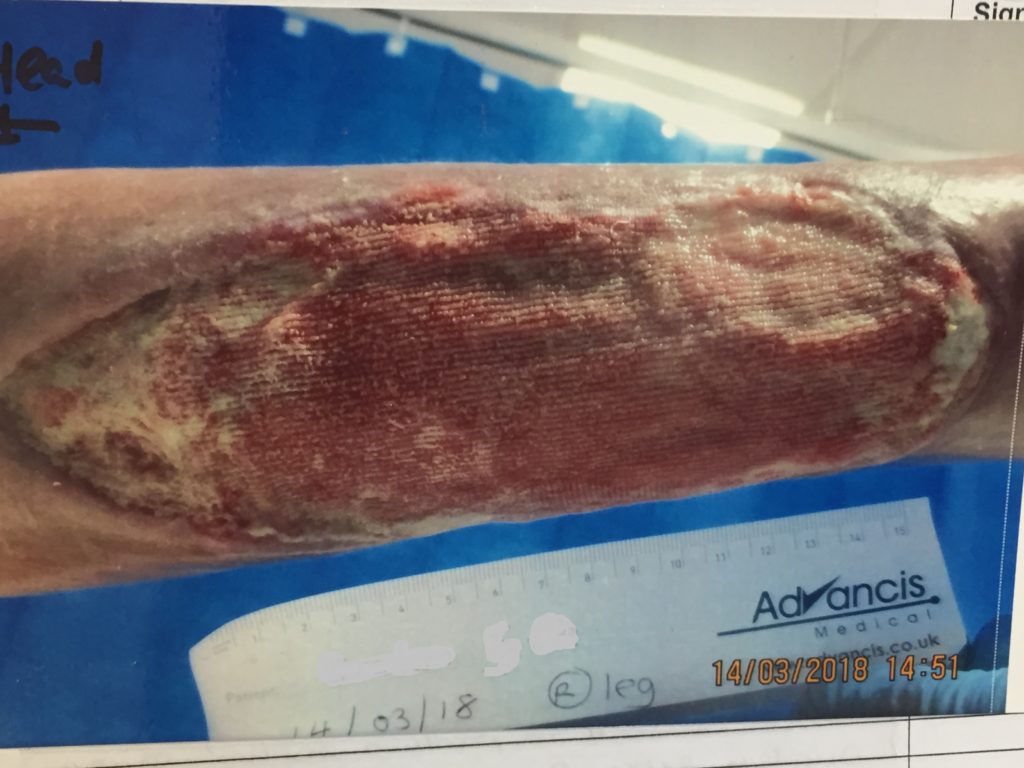
End of week one
By the end of week one, all of the necrotic tissue had debrided. There was no change in the length and width of the wound but it was now shallow with healthy granulation tissue and intermittent areas of slough to both the distal and proximal ends of the wound. Undermining to the proximal aspect of wound had almost resolved. Mr C reported an improvement in his pain levels. He was keen to go home and, following an assessment with the Plastic Surgeon it was agreed to discontinue the V.A.C. VERAFLO™ Therapy and recommence NPWT using ACTIV.A.C.™ Therapy system with V.A.C.® GRANUFOAM™ Dressings with the prospect of the patient having a skin graft at a later date.
Mr C’s pain was now under control and he was mobile with the use of with a wheelchair and partially weight-bearing with crutches.
At the point of discharge, Mr C was discharged to home with an ACTIV.A.C.™ Unit. A referral was made to the District Nurses to continue with on-going management of the wound and he was to be reviewed by the plastic surgery team as an outpatient.
Several months later, Mr C was readmitted to hospital. His wound had not fully healed but was smaller and being managed with conservative dressings. He had fully regained his mobility and was independent with all activities of daily living.
Had we not commenced the V.A.C. VERAFLO™ Therapy there is a very real chance that this gentleman would have required an above knee amputation. This would have affected every aspect of his life from the obvious physical and psychological effects to social implications such as adaptations required to his home. Application of the V.A.C. VERAFLO™ Therapy dramatically improved Mr C’s wound in a short space of time and as a result reduced the length of his hospital admission by several weeks, allowing him to regain full independence again.