Case Study
Authors:
Traïka Desmet, Heidi Weedaege: Wound care nurses, Belgium
Introduction:
On November 20 2019 a 86 year old female is admitted due to a wound on the left lower leg (more specifically the calf).
The injury was considered as a complication after a locoregional anesthetic technique (popliteal block), possibly caused by the puncture or possibly a spontaneous bleeding. The exact cause of the bleeding is unknown.
Methods:
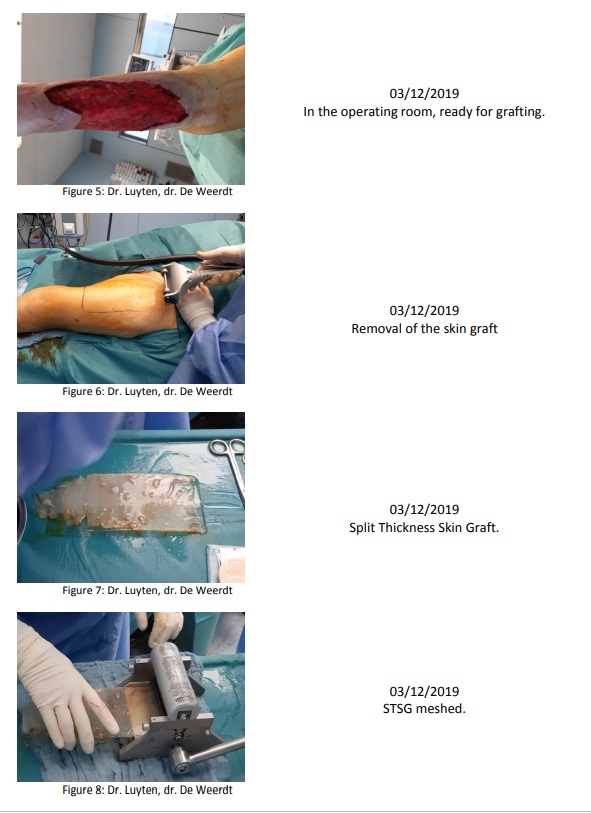
The aim was to achieve a successful debridement in order to continue with normal V.A.C.
granufoam dressings to result in a granulating wound ready for grafting.
Results:
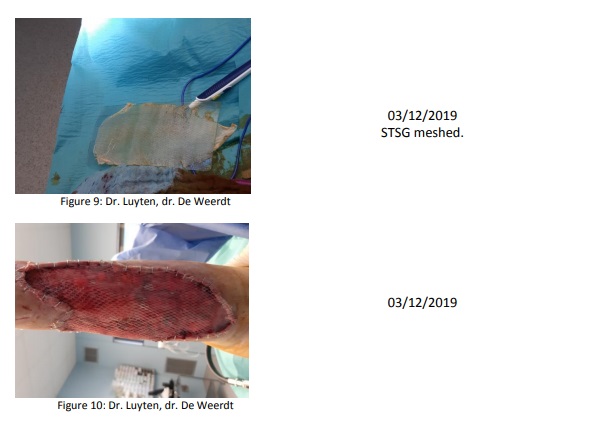
A successful debridement was achieved as well as a reduction in the bacterial load, in only a couple of days, so that the wound could be grafted after a short period of time. Various narcosis could be avoided for this patient with different comorbidities.
In addition to the care of the wound, we saw the patient was comfortable with the therapy. She experienced a lot of pain during the care, which made her anxious and experiencing stress. Before the dressing changes, a pain protocol was drawn up in consultation with the treating physician.
Discussion:
We have only recently got to know the dressing so we are careful in our conclusion, multiple applications in different indications are needed.
Conclusion:
The V.A.C. Veraflow™ with the Cleanse Choice Dressing was successful in this case.
Patient history:
On November 20, 2019 a 86 year old female was presented with an injury on the calf of the lower limb.
She has been treated and followed up for type 2 diabetes. She has a history of vascular suffering. In 2000 she was affected by a stroke (TIA). She has also developed chronic renal failure.
Due to these comorbidities and the resulting problems she has her first vascular surgery of the lower limb due to arterial insufficiency on July 5. A percutaneous transluminal angioplasty of the arteria femoralis superficialis, arteria poplitea, arteria fibularis and arteria tibialis anterior was performed. After four months her doctor observed an injury to the
fourth toe of the left foot. A revascularization procedure of the arteria femoralis superficialis and the arteria poplitea was performed on November 8 along with a debridement of the toe. Four days later the wound to the toe deteriorated. So on November 13 the toe was amputated because osteomyelitis was present. This procedure was performed under a locoregional anesthesia, a popliteal block. A major subcutaneous
bleeding occurred one day after the procedure, possibly by puncturing for anesthesia, possibly spontaneously (Fig.1).
On November 18, the hematoma was drained and necrotic skin removed in the operating room (Fig.2). After this surgery wound care was prescribed with Iso-Betadine® gel (PVP-I).
The wound nurse was asked in consultation.
The Cleanse Choice Dressing and V.A.C. Veraflow™ was applied on November 21.
The therapy settings:
– Negative pressure: 125mmHg
– Instillation volume: 30 cc
– dwelling time: 5 min
– V.A.C. therapy: 3 h
– instillation fluid: saline
Two dressings were needed: the first on November 21 and the second on November 25.
After evaluation, the wound was found well that therapy was switched to ActiV.A.C. on November 29.
And finally on December 3 the wound was grafted (Fig. 10). A first wound check will be done on December 9 by the plastic surgeon.