Case Study
Case Study
Infected Caesarian section wounds are not particularly unusual. This report, however, highlights one such wound, which was more complex than usual and discusses the unique management style employed at the Cape Advanced Wound Care Centre. The “Debridement, Optimisation and Surgical Closure” method used has proved successful in most patients treated at this facility.
Introduction
This case was unique as many of these types of wounds can become very costly and could potentially proceed to even more serious complications if not treated appropriately. This is particularly a case that sparked an interest to me as I realized how crippling this could be to a patient. When I think of the fact that a mother that is breastfeeding, having a newborn child and must deal with a wound now as well. The psychosocial, emotional, psychological and economic impact that this has on a patient and patient family.
Informed consent was obtained from the patient for this case study presentation.
Patient background and Case Presentation
The patient is a 37-year-old female that had a Caesarean section in April.
She is a young woman that does photography as an occupation and has no known history of any other co morbidities. This was her third pregnancy and she had no complications with her first two pregnancies.
One week post operatively the wound showed signs of infection as the wound developed a “pimple“, and the surrounding skin became erythematous. The wound later started exuding pus after attempts were made to express the contents of the “pimple” at the local wound clinic. A plastic surgeon was consulted two weeks postoperatively.

The surrounding skin, about 3cm long on the left flank of the lower abdomen, showed signs of erythema and the plastic surgeon informed the patient about the surgical approach that will be taken.
Initial Treatment and Actions.
During the surgery the doctor found a considerable amount of necrotic fat beneath (Figure 2) the skin. This was debrided using a commercially available hydro debriding device. (Figure 3)
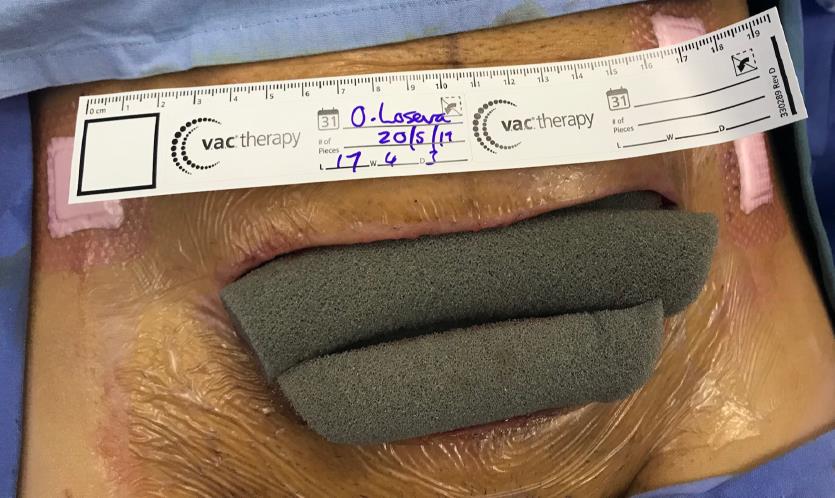
A polyvinyl alcohol (PVA) white foam NPWT (AcelityTM, San Antonio, USA) was place into the cavity and
connected to a NPWT portable unit. The patient was scheduled for follow up NPWT changes with the Private
Nurse Practitioner.

Kairinos

the PVA NPWT. Courtesy Dr Kairinos

into this debrided cavity. Courtesy Dr Kairinos
Progress of the treatment for this patient.
Three days after the initial surgical intervention the patient went to see the Nurse Practitioner for a wound check and dressing change. While doing the NPWT dressing change the Nurse Practitioner noticed the presence of pus from the wound edge. The Plastic surgeon was informed about the observations and the surgeon requested diagnostics tests.
PVA NPWT was continued and on the third dressing change the patient complaint of feeling feverish and still pus present from the old suture line.
An Ultrasound of the abdomen and pelvis was done and revealed no intraperitoneal abscess collection but mentioned a possible liquefied hematoma.
Microbiology had a Gram-Positive Cocci which was then treated accordingly with antibiotics.
The wound show improvement with the NPWT PVA dressings changes. Two weeks later with this treatment, the wound was ready for closure as seen in Figure 5 below.
While performing the scar excision, the doctor noticed multiple pus pockets extending to and including sheath fascia. The pus extended to the midline, but the doctor propped sheath and it did not appear to have
gone intra- abdominal. Wound was cleaned in theatre and then elected not to close the wound. Now the NPWT with Installation (NPWTi) was applied. (Figure 6,7)
NPWTi was used to deliver 40ml Saline with a 6min soak phase and 3.5 hours V.A.C.® Therapy phase by using the Medium Cleanse Veraflo kit. (Figure 8,9)
The wound was treated with this NPWTi but with the dressing change we noticed that it seems like the wound base did not appear to have granulated well and there was an odor still present.
Upon changing the NPWTi, the Fill Assist on the Ulta machine was utilized and now managed to instill 120ml of Saline instead of 40ml into this wound.

Courtesy Dr Kairinos

Courtesy Dr Kairinos

and NPWTi inserted. Courtesy Dr
Results and Closure of this wound.
After four session with the NPWTi the patient was brought back to theatre for the closure of the wound. The doctor closed the wound by having the skin edges excised, upper abdomen flap released and brought down
for closure procedure. (Figure 10) This technique was used and as the patient had complications with her wound, which resulted in extensive debridement sessions, the Prevena Short (AcelityTM, San Antonio, USA)
incisional NPWT system was applied to the skin. These devices have been shown to reduce wound complications in high-risk wounds.3 (Figure 11)
The wound was closed, and she came for follow up four days later and the Prevena was removed and the wound did well with the Prevena on it and then conventional dressings was used over the suture line. Wound was inspected several times after, and the suture line healed. Two weeks after the closure the wound was only using skin tone micropore over the suture line. (Figure 12)

Kairinos

Courtesy Dr Kairinos

Courtesy Dr Kairinos
Discussion
With NPWTi this wound from the start would have progressed must faster than Core NPWT but with this case the pockets of pus only showed up when the wound was ready for closure.
If this wound would have been treated with the series of NPWT and then moved to conventional wound care, the pus and necrotic tissue under the skin would not have been discovered. This would have developed
into much more serious complications.
This is important that patients with complications and the complexity of such wounds, should be referred early to Centre that can deal with such complex wounds.
“Using this approach has yielded favourable results, with most patients experiencing wound closure times that are a fraction of the time that the wound was present prior to presenting at the wound care center. There are multiple benefits to this accelerated regimen, including psychological, financial (for the patients and medical funder) and the physical well-being of the patient. Having patients return to work earlier is an obvious
benefit to the country as a whole.2”
Clinical Outcomes/ Conclusion:
This wound took five weeks to completely close from the initial assessment when she came to this facility. This was already two weeks post her Cesarean section. Due to her complications after the delivery the patient was treated in total for seven weeks. If the team approach was not done with this case in combination with the NPWTi this could have led to serious complications.
This is important to deal with these complex wounds as soon as possible especially when there is signs of wound infection or dehiscence. If this patient was referred sooner this could have been dealt with sooner
and would potentially have been closed sooner as well.
As per Gabriel A, (2008) NPWT instillation showed a significant decrease in the meantime to bioburden reduction, wound closure and hospital discharge compared with traditional wet-to-moist wound care.1
The use of NPWT instillation and having a team approach may help in reducing the cost and decrease inpatient care requirements for these complex, infected wounds.

Courtesy Dr Kairinos
Reference:
- Gabriel A, Shores J, Heinrich C, Baqai W, Kalina S, Sogioka N, Gupta S, 2008, Negative pressure wound
therapy with instillation: a pilot study describing a new method for treating infected wounds.
International Wound Journal; 5(3):399-413. - Kairinos N, 2019, Woundectomy, multidisciplinary wound care and closure – the most effective way
to treat complex wounds. Wound Healing Southern Africa 2019 Volume 12 No 1 - Willy C, Agarwal A, Andersen CA, et al. Closed incision negative pressure therapy: international
multidisciplinary consensus recommendations. Int Wound J. 2015; 14(2):385-398. - Consent form