Case Study
MANAGEMENT OF A PATIENT WITH AN INFECTED BELOW KNEE AMPUTATION STUMP USING VAC VERAFLO THERAPY
Published: November 18, 2019
Authors: Natalja Grohmann, Sabine Stasko
Department of Vascular Surgery, Klinikum St. Marien, Amberg
CASE STUDY
We report on a 62-years-old male patient with a case of PAD-related right below knee amputation, diabetes mellitus, art. hypertension, nicotine abuse and hypercholesterolemia.
The patient was admitted to our department due to a worsening of below knee amputation wound. The clinical examination showed a black necrotic, mainly dry, amputation wound. Subcutaneous pocket formation on the medial side of the stump with a turbid exudate and stinking secretion. So that a surgical revision of the amputation stump was indicated.
The procedure was carried out after appropriate preoperative preparation. The operative finding after excision of the necrotic tissue from the medial wound area was plenty of pus emptied from the cavity. The abscess cavity (depth approximately 2,5 inches) was opened, rinsed and refreshed with a sharp spoon. The avital muscle tissue was excised without reaching the bone or periosteum.
Subsequently, a VAC.ULTA with 75 mmHG negative pressure was applied continuously. After the first change of VAC, necrotic tissue appeared again in the medial wound area. That\’s why we decided for maggot therapy to dissolve the necrotic tissue. On the next day, because of a lot of foul-smelling exudate, causing the larvae to drown, we stopped the maggot therapy and started the VAC VeraFlo therapy. As irrigation solution Granudacyn was chosen. The VAC therapy time was 3 ½ hours, the Granudacyn exposure time 2 minutes at 75 mmHG negative pressure setting. After regular VAC changes (twice a week) avital tissue was successively removed localy with a scalpel. The procedure took place on our ward. A steady improvement of the wound situation was visible with each change of VAC. The total treatment with VAC VeraFlo was 33 days. The tissue became more vital and the total size of the wound smaller.
At this stage we were able to discharge the patient home with acti-VAC with the prior approval of the health insurance company.
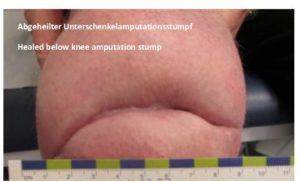
The acti-VAC was continued for 20 days with great success and then ended and further conservative wound dressings were recommended. Two weeks later, the patient showed a completely healed below knee amputation stump.










Conclusion:
The VAC-VeraFlo therapy is according to our experience a very useful treatment method especially for deep, infected wound cavities or abscess cavities lead to an irrigative cleaning of the wound surface and thus a reduction of the bacterial load.
Using this method enabled us to avoid excessive intraoperative deep surgical debridement with eventual bone exposure. In our case the below knee amputation stump was preserved and a high level amputation was avoided.
It is worth mentioning that during the VAC VeraFlo therapy, the patient always stayed independent and mobile through a self-created device, which he built for his wheelchair to attach the VAC.ULTA.