Case Study
NPWT i-d IN COMBINED SURGICAL TREATMENT FOR FOURNIER’S DISEASE
Baglioni E.A MD§, Destefanis P. MD PhD *, Isaija I M.D. §, Russo A. #, Gianfala A. M.D§, Bernuzzi E M.D §, Bruschi S M.D. and Bocchiotti M.A. M.D.§.
§ Plastic Surgery Department, University of Turin
Città della salute e della Scienza di Torino
*Urology Department, University of Turin
Città della salute e della Scienza di Torino
# Nurse expert in wound care, UCQP , Health Directorate
Città della salute e della Scienza di Torino
INTRODUCTION
Fournier’s gangrene is a rare, potentially life-threatening, rapidly progressive and necrotizing soft tissue infection of perineal, genital and perianal region [1]. It is associated with a high morbidity and mortality rate ranging from 3 to 67%. In most cases is a poly-microbial infection that causes thrombosis of vessels leading to tissue ischemia. Ischemia promotes infectious dissemination and induce skin necrosis.
The infection involves aerobic and anaerobic organism originating from a urogenital, colorectal or cutaneous source.
Men are involved more frequently than women, and the highest incidence occours in the sixth decade. The predisposing factors are diabetes mellitus, alcohol abuse, immunodeficiency, malignant neoplasm, liver and renal diseases.
An aggressive and early treatment is very important for the survival of these patients. The mainstay of treatment consists of radical excision of necrotic tissue, broad-spectrum antibiotics, intensive care and nutritional support.
We describe a case of extensive Fournier’s gangrene treated with Veraflo (KCI, Acelity, S. Antonio Texas) and Vac Therapy in concert with surgical debridement.
CLINICAL CASE
On February the 27th 2018 a 65-year-old male patient with uncontrolled diabetes, obesity and hypertension presented to the emergency room with high fever, confusional state displaying edema, ecchymosis and initial signs of necrosis of perianal region, scrotum and pubis (FIG. 1). The patient was admitted to intensive care unit. He began antibiotic therapy with daptomycin, clindamycin, meropenem and metronidazole.
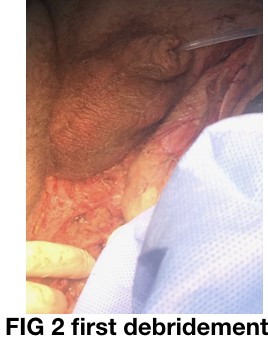
The patient was taken to the operating room to undergo in emergency surgical debridement of the necrotic tissue along with the urologist. A Y-shaped incision was made in the perianal and scrotal region to remove the necrotic and infected tissue, thus leaving the spermatic cord and left testis exposed (FIG. 2-3).
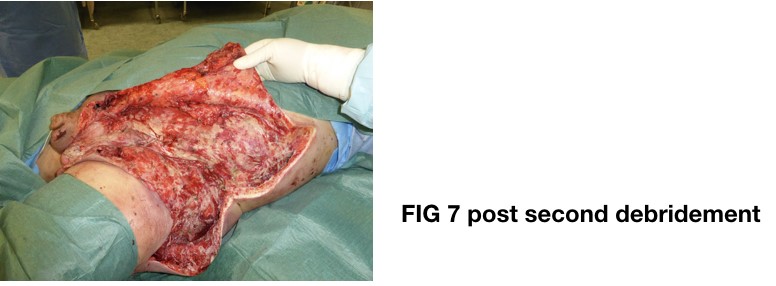
On the second postoperative day general condition worsened with extending edema and redness of the left upper thigh and the lower abdominal regions along the anterior axillary line. WBCs count was 39.000, CPR value was 390 and Procalcitonin value was 31. The patient was in septic shock. The plastic surgeon made incision on the lateral aspect of upper thigh up to the left flank with extensive debridement of necrotic subcutaneous and fascial tissues. The patient was medicated with antiseptic gauzes containing biguanid (Kerlix – covidien). A left colonstomy for faecal diversion was performed (FIG. 4-5-6-7).
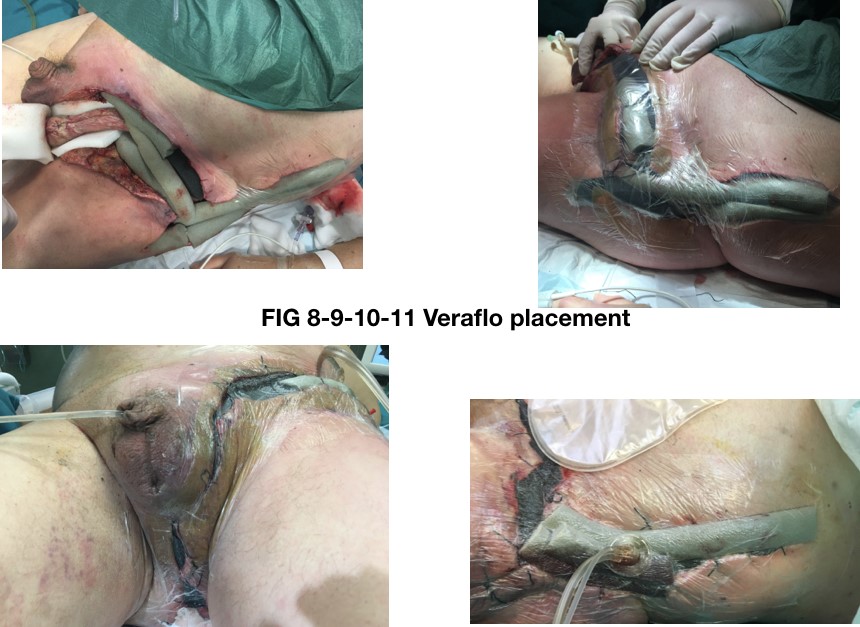
On the third day from admission the patient underwent further surgical debridement of the remaining necrotic tissue and Veraflo device was applied in collaboration with wound care APRN to cleanse the wound bed and promote granulation. The medication was made with two large plus two medium veraflo dressing kits and Veraflo Cleance dressing kit. Spermatic cord and left testis were sheltered with White-foam. Medication was kept in place by 0 silk sutures in the scrotal, perineal and sovrapubic area [2]. A gauze with VAC-adhesive was inserted in the anal canal to avoid leak. NPWTi-d settings were 200 ml of Polyhexanide (polyaminopropylbiguanide) + Betaine 0,1% as irrigating solution, 15 minutes of dwell time with cycle frequency of 4 hours at costant negative pressure of 150 mmHg (FIG. 9-10-11)
Blood coltures were positive for Escherichia coli. Wound swab colture was positive for Streptococcum costellatum, Enterococcus faecalis, and Bacterioides thetaiotaomicron.
The patient was treated with Veraflo for 20 days from March the 1st 2018 to March the 20th with dressing replacement carried out twice a week under heavy sedation.
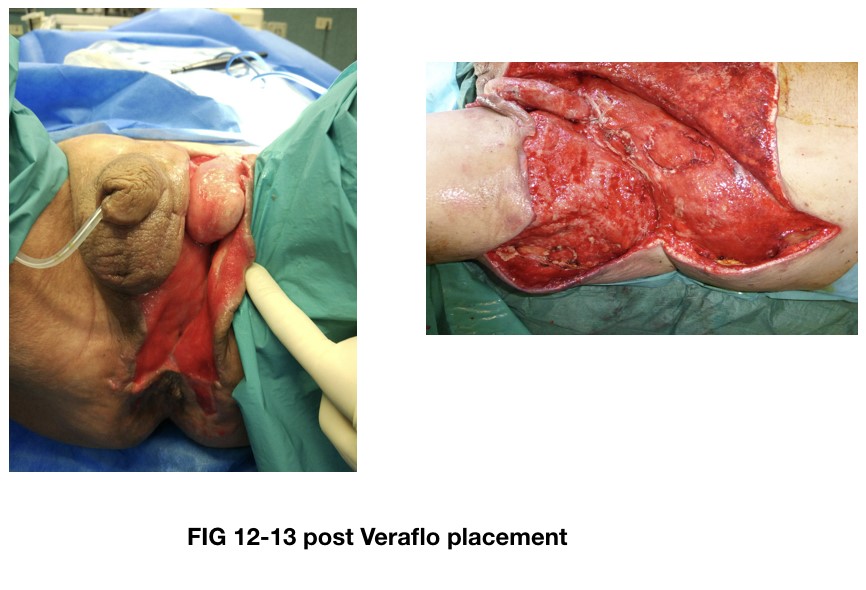
On March the 24th the patient was transitioned to NPWT with granufoam medium dressing kit (6 pieces) and white foam on the spermatic cord and testis (FIG. 12-13). Dressing replacement was carried out twice a week. The application of VAC therapy was associated with antiseptic gauzes containig biguanide (Kerlix – Covidien) on the following 7 days.
In early April the 3rd his clinical condition bettered so that he was moved to long-term ward.
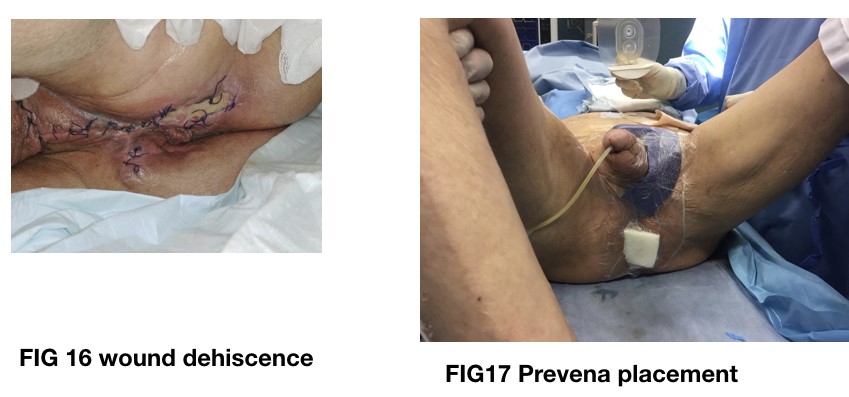
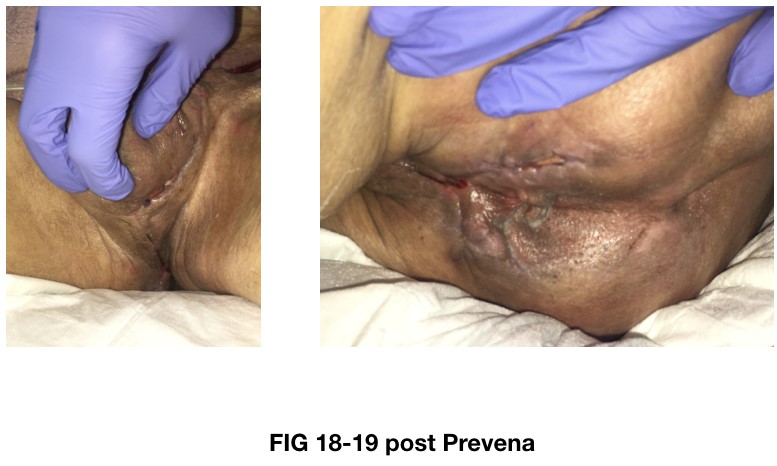
After 15 days of VAC-therapy on April the 4th the left testis and spermatic cord were replaced in their proper anatomical site and the wound along the perineal, scrotal, inguinal and sovrapubic region was surgically closed. He went on with application of VAC-therapy at abdominal site under sedation in operating room twice a week with progressive reduction of the extent of tissue loss (FIG. 14-15). 7 days from inguinoscrotal wound closure in occasion of the dressing change initial dehiscence with serous discharge was observed. In order to prevent further dehiscence of the suture a Prevena medication was placed on the sutured area and granufoam simplace dressings was placed at the abdominal site with only one VAC-ulta device providing 150 mmHg of negative pressure (FIG. 16-17-18-19). Prevena medication was removed on April the 27th after 15 days of NPWT with no signs of dehiscence. By means of VAC-therapy progressive attachment of the cutaneous and subcoutaneous flaps was achieved. At the time the tissue loss measured 25×8 cm with healthy granulations. On May the 2nd the patient underwent split-thickness mesh graft from the anterior aspect of the right thigh to cover the residual tissue loss. VAC-therapy with white foam was placed for 7 days over the grafted area to absorb serous discharge and to promote engraftment (FIG. 20-21-22-23) [3-4].
On May the 8th VAC-therapy was removed showing skin engraftment up to 80%. Hydrofiber dressings with silver and polyurethane foam were applied and periodically changed until complete healing. On may the 29th the patient was discharged.
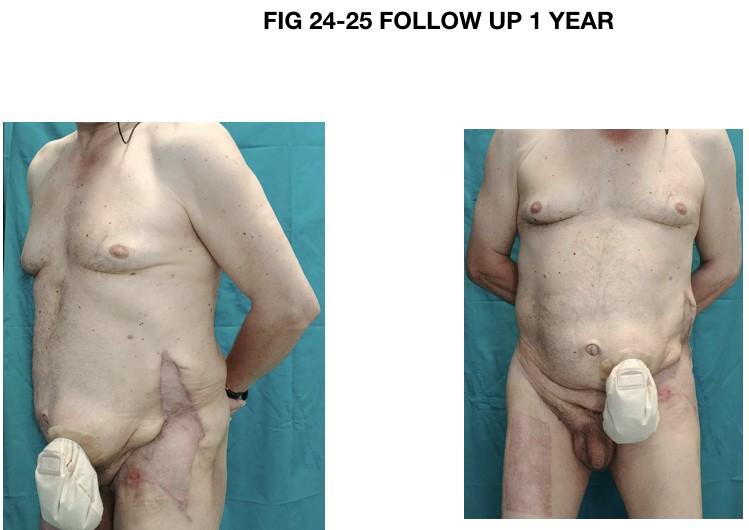
The wound healing was achieved in 90 days. The patient was followed with outpatients appointments up to 12 months after surgery. No complication occurred during the follow-up period. One year from discharge he showed good functional outcome with no wound healing defects and scar contracture either in perineal region or in scrotal region. The engrafted area still appears dyschromic (FIG. 24-25).
DISCUSSION
In this case the multimodal aggressive approach to Fournier’s gangrene (debridement, antibiotic therapy, resuscitation care, nutritional support) allowed the patient to survive. The use of the NPWTi-d achieved the removal of necrotic debrides and clearance of the infection and decreased the tissue edema. The subsequent use of NPWT increased the granulation of the wound, reduced the dimension of the tissue loss promoting the attachment of the wound flaps. The experience of the health care professionals along with the development of new technologies allowed complete healing of the wound with minimal relics and no functional deficiencies. This result was achieved by using different kind of filler foams chosen according to the wound bed state and the stage of the wound healing process.
The association of NPWT and NPWTi permitted the closure of the wound with a simple skin graft because the residual tissue loss was superficial and of reduced extent compared to the initial tissue involvement. The Veraflo promoted wound bed cleansing preventing the infectious necrotic process to reach the abdominal fascia thus avoiding the involvement of the endoabdominal organs and subsequent risk of visceral herniations.
According to the latest global guide lines it is advisable to use Veraflo in association with surgical debridement to cleanse complicated wounds not only to remove infectious tissues but also because a wound of such extent as the one described above, if left open, exposes the patient to a greater infectious risk and to increased perspiration [5]. This confirms the superiority of NPWT over conventional dressings [6].
REFERENCES
1)Yanaral F., Balci C., Ozgor F. et al. Comparison of conventional dressings and vacuum-assisted closure in the wound therapy of Fournier’s gangrene. Archivio italiano di urologia ed andrologia 2017:89,3
2) Chang et al. Suture Technique to Prevent Air Leakage during Negative-Pressure Wound Therapy in Fournier Gangrene. Plast Reconstr Surg Glob Open. 2018 Jan 25;6(1)
3) Tian Y, Liu T, Zhao CQ, Lei ZY, Fan DL, Mao TC. Negative pressure wound therapy and split thickness skin graft aided in the healing of extensive perineum necrotizing fasciitis without faecal diversion: a case report. BMC Surg. 2018 Sep 24;18(1):77.
4) Alwaal A, McAninch J, Harris C, Breyer B. Utilities of Split-Thickness Skin Grafting for Male Genital Reconstruction. Urology . 2015 Oct; 86(4):835-9
5) Kim P.J., Attinger C.E., Constantine T., Crist B.D., et al . Negative pressure wound therapy with instillation: International consensus guidelines update. Int. Wound J. 2019;1-13.
6) Yanaral F. et al. Comparison of conventional dressings and vacuum-assisted closure in the wound therapy of Fournier’s gangrene. Arch Ital Urol Androl. 2017 Oct 3;89(3):208-211