Case Study
Introduction.
V.A.C. Verafloä Therapy is a well-known and quite well-established therapy in treating diabetic foot ulcers (DFU). It is known that the NPWT therapy with instillation improves the wound healing of granulation tissue. Especially in our department the `normal` V.A.C.â and the Verafloä therapy are used very often to treat DFU and other vascular wounds.
Methods.
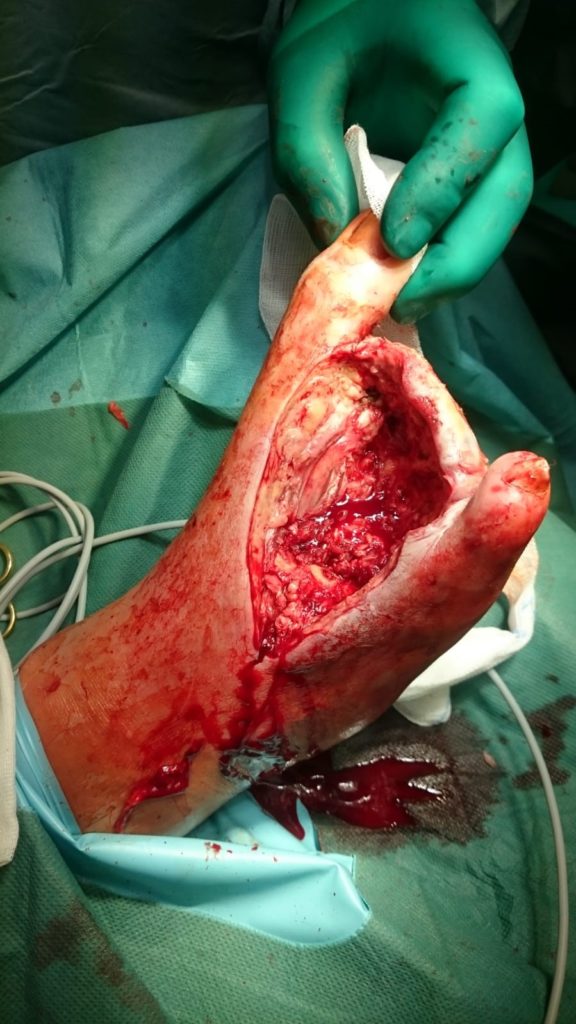
In the following case study, there is a 67-year-old male patient with a gangrene in the foot and a sepsis. He came to our emergency department with a gangrene in the foot (Figure 1), a temperature of 38°C and a CRP of 308 mg/l (standard value < 5mg/l). He had a diabetes for many years (more than 20) and besides that a Korsakov syndrome because of alcohol, but no further illnesses.
At first, we started with antibiotics (Unacid) and did an emergency operation in order to treat the sepsis. Originally, we planned a major amputation of the lower limb but decided to try a minor amputation and a necrectomy at first (Figure 2).
On day 3, we started the V.A.C. Verafloä therapy with our standard setting (instillation liquid: Lavanidâ, dwell time: 15 min, V.A.C. time 120 min, 125mmHg). After emergency operation, antibiotics and Veraflo therapy, there was a decrease of the CRP to 6.9 mg/l on day 13. Unfortunately, there was an increase of necrosis so that we had to amputate the fifth toe, as well. Due to increased necrosis, we started the V.A.C. Verafloä therapy with the cleanse choice dressing and our standard setting for this therapy (instillation liquid: Lavanid â, dwell time: 15 min, V.A.C. time 90 min, 125mmHg) on day 19 (Figure 3).
Due to this therapy, there was less necrosis and an increase of granulation tissue after only 3 days (Figure 4). After some renewals we could de-escalate to `normal` V.A.C.â therapy on day 31 (Figure 5) in order to consolidate the ground of the wound for a skin graft (Figure 6).
Finally, we did the skin graft on day 35 and applied the V.A.C.â therapy for five more days (100 mmHg) in conformity with our standard (Figure 7). Thus, the patient could be discharged on day 42 after removing the clips. Unfortunately, he didn´t show up for the follow-up.
Discussion.
In this case, the NPWT with instillation decreased necrosis extremely effectively, and- together with systemic antibiotics – local infection as well. Furthermore, the Verafloä therapy was able to increase granulation tissue very impressive. De-escalation is executed for economic reasons. As a consequence, we developed a `de-escalation system’ as follows: Use V.A.C. Verafloä with cleanse choice dressing to remove necrosis and debris. De-escalate to `normal` V.A.C Verfloä therapy to treat infection and biofilm, as well as to give the first impulse for granulation. When the wound is clean and it granulates, de-escalate to `normal` V.A.Câ therapy.
Result.
In conclusion, by using NPWT with instillation together with systemic antibiotics and operation, we could prevent a major amputation and could discharge the patient after 42 days from hospital. Furthermore, we considered economic values by using our de-escalation system.
Reference.
Harzklinikum Wernigerode, department of vascular and endovascular surgery, Wernigerode (Saxony-Anhalt), Germany, Dr. med. T. Mildner (head of the department)