Case Study










V.A.C. VeraFlo™ Therapy with three different types of fillers in temporal succession: V.A.C. VERAFLO CLEANSE CHOICE™, V.A.C. VERAFLO CLEANSE™, V.A.C. VERAFLO™ Dressing
Post-Traumatic Necrotizing Fasciitis and infected wound
Colognese Stefano, Wound Care Specialist RN MSc
Azienda USL, Presidio Ospedaliero ASMN-IRCCS, Reggio Emilia, Italy, IT
On January 22nd 2019 traumatic event: pedestrian hit by car.
A 81-year-old female is hospitalized in Intensive Care Unit for polytrauma with a reserved prognosis. Subjected to CT and traditional radiology, she presents: sub arachnoid hemorrhage, head trauma, thoracic trauma with multiple rib fractures, spinal trauma and vertebral fractures, trauma and fracture of the pelvis in multiple locations, multiple fractures in the left arm and forearm, multiple fractures to the femur and leg both on the right and on the left.
On February 8th 2019 I was contacted by orthopedic surgeons for the assessment and treatment of complex wound: extensive cavitary lesion on the right thigh, medial side. There is a wide undermining (detachment) between 12 and 4 hours, detected with sterile specimen and clock/position technique. Already performed debridement by the orthopedic surgeon (who removed most of the necrotic tissue). The wound bed presented slough, yellow-black necrosis, and infection. The exudate was abundant and purulent (dense, viscous, turbid, milky), yellow-brown in color, smelly. The edges were necrotic, jagged, irregular, undermined (detachment), rounded, rolled and blocked. The perilesional skin was reddened, macerated, hot, with the presence of edema and cellulitis. The lesion had an area of 59.0 cm2. Culture tests (blood cultures, deep biopsies, bronchial aspirate) were positive for infection (Elizabethkingia meningoseptica, Enterobacter cloacae, Proteus vulgaris group, Acinetobacter spp, Stenotrophomonas maltophilia). Figure 1/1a/2
At first the wound was cleaned with a 0.05% sodium hypochlorite-based solution using a cavity pack held in place for 10 minutes.
An NPWTi with V.A.C. VERAFLO CLEANSE CHOICE™ technology was therefore positioned, according to the following method: 1) protection of perilesional skin with 3M™ Cavilon™ (protective film in liquid form), 2) additional protection of perilesional skin by packaging of \\\”dam\\\” (Advanced Drape – sterile transparent adhesive film), and exposure of the wound bed, 3) Filler: V.A.C. VERAFLO CLEANSE CHOICE™ Dressing – Medium, cut and shaped in mold, 4) Sealing of the Filler with V.A.C. Advanced Drape (sterile transparent adhesive film), and further reinforcement of the system with the same material (included in the Kit), 5) Central positioning of VeraT.R.A.C., 6) Type of solution instilled: 500 ml of Physiological Solution + 500 ml of 0.05% Sodium Hypochlorite, 7) Instillation volume: 100 ml per cycle (every 3 hours, for a total of 8 washes in 24 hours), 8) Infiltration time: 10 minutes, 9) Duration V.A.C. Therapy: 3 hours post-infiltration, 10) Target Pressure: 125 mmHg, 11) Intensity: Medium, Device: V.A.C.Ulta™ motor unit, Canister: V.A.C.Ulta™ (1000 cc). CHANGE MEDICATION: EVERY 3 DAYS.
After 3 days (on February 11th, 2019), the wound bed was well cleansed with abundant tissue growth. The exudate was moderate, serum-ematic, not smelly. The perilesional skin was still a little red but less edematous. It was therefore decided to continue the cleansing and decontamination of the wound, changing only the type of filler (V.A.C. VERAFLO CLEANSE™): the treatment method has remained unchanged. Figure3/3a
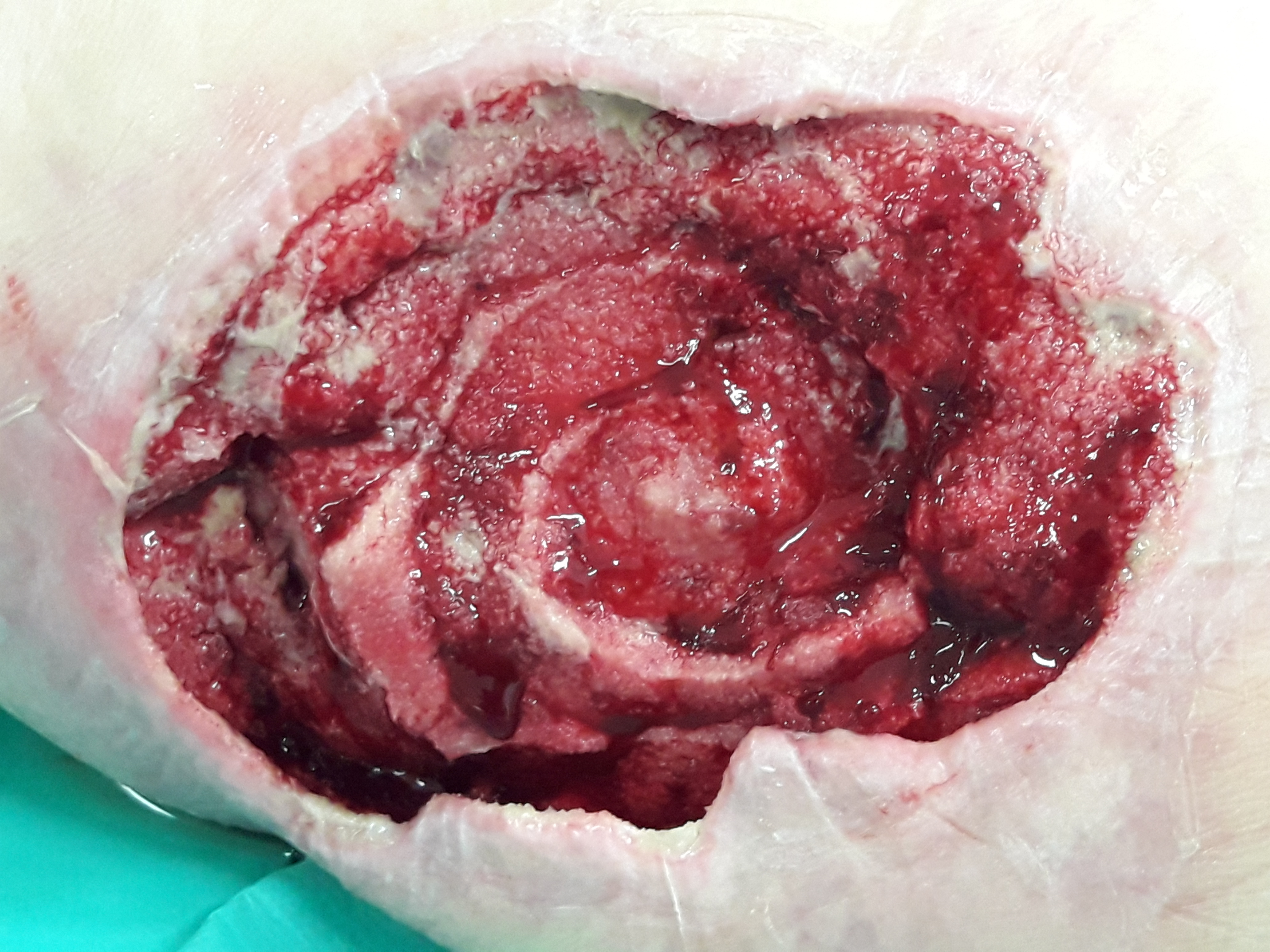
After 6 days (on February 14th, 2019), the wound bed appears completely cleansed with abundant presence of richly vascularized granulation tissue. The perilesional skin is now normothermic, not reddened, not edematous and even the cellulitis is completely regressed. All the indexes of inflammation and infection were in rapid regression. It should be noted that the granulation tissue was grown adapting and modeling itself to the filler morphology (V.A.C. VERAFLO CLEANSE™). Obtained the optimal cleansing and decontamination of the wound bed, the primary objective was to favor the growth of the granulation tissue, homogenizing both the volume and the surface of the lesion: the filler was then changed again, choosing V.A.C. VeraFlo™ Dressing. Also in this case the same treatment settings were maintained. Figure 4/4a
After 13 days (on February 21st, 2019), the loss of tissue substance had been completely recovered and the wound bed almost completely homogenized. The edges were active, on approach, with the presence of re-epithelialization areas. Even the undermining had been completely reabsorbed. No local signs of infection present. Figure 5/5a
On February 22nd 2019, during the transfer of the patient to a respiratory rehabilitation center, the treatment with V.A.C. VeraFlo™ Dressing has been closed, and the wound has been managed with advanced dressings. It was not possible to follow the evolution of the lesion. However, a follow-up was carried out on May 16th 2019 when the patient requested an evaluation in the Structure of the Wound Care Specialist (Colognese Stefano). The lesion was completely closed with a scar during remodeling. Further follow-up was carried out on November 26th 2019. Figure 6/7
Conclusions: ”The overview and literature analysis suggest that NPWTi is, in certain clinical situations, more beneficial than standard NPWT for the adjunctive management of acutely and chronically infected wounds that require hospital admission**”, “Additionally, there are clinical observations that NPWTi by saline is more effective in wound healing that NPWT alone**”.
My clinical experience related to the use of V.A.C. VeraFlo ™ Therapy suggests that, based on wound bed conditions and treatment goals (debridement, cleansing, decontamination, granulation tissue growth), the most appropriate filler should be chosen. The management of this clinical case has clearly demonstrated that by varying the type of filler according to the evolutionary moment of the lesion, the use of NPWTi significantly reduces treatment times with an early achievement of pre-set outcomes. Figure 8
Evolution of the wound bed in 13 daysFigure 8. Evolution of the wound bed in 13 days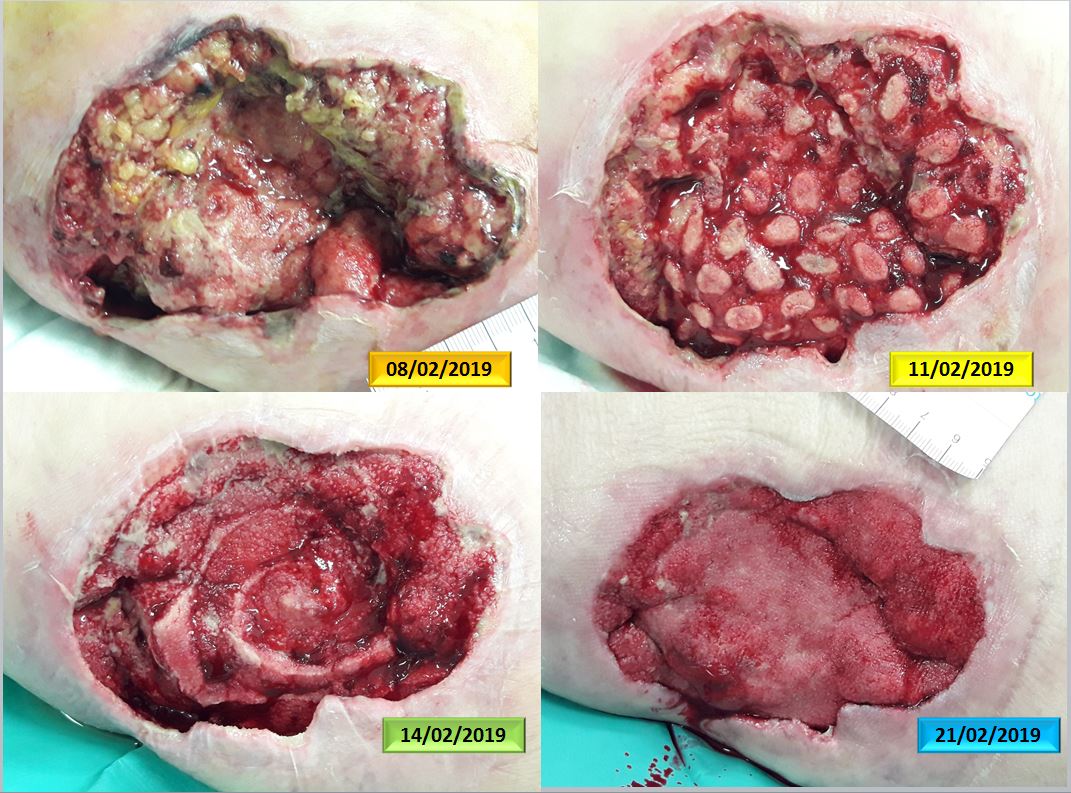
**Apelqvist, J., Willy, C., Fagerdahl, A.M. et al. Negative Pressure Wound Therapy – overview, challenges and perspectives. J Wound Care 2017; 26: 3, Suppl 3, S1–S113.
