Case Study
Institution: Gza hospitals
City/Country : Antwerp, Belgium.
Koen Cortebeeck, wound care nurse,
Declaration of Interests
The author declares that he has no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
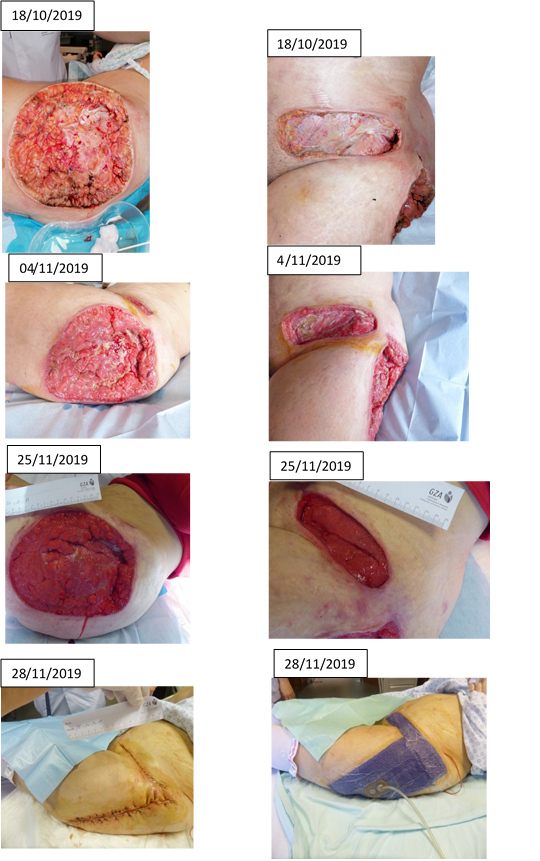
Case Presentation This case concerns a 35 year old patient with ecchymosis lateral above the groin, large necrosis laterally above the thigh and elevated wound edge.
Pre- existing co-morbidities included; 2006 auto immune hepatitis, 2015 Lupus, 2017 confirmation systemic lupus erythematosus, 2018 Cirrhosis as a consequence of auto immune hepatitis.
13/10/2019 An urgent surgical debridement was considered necessary .
The wound culture shows Streptococcus pyogenes type A. Necrotizing fasciitis.
A relook was done the 14th of October with additional debridement of the wound edges.
Antibiotics were adjusted to high-dose penicillin and Dalacin®
Because the patient was immunocompromised, it was necessary to administer immunoglobulins for 3 days.
Levophed® was started to treat the shock. Medrol® 4g was administered to treat the autoimmune reaction.
No additional necrosis was observed the following days. The wound was not completely clear of infection and had to be treated.
A negative pressure system with VAC Veraflo® was placed on the 18th of October.
The wound bed at the height of the thigh was very irregular, due to the presence of fat tissue.
We used a negative pressure of -125mmHg. As instillation solution we used povidone iodine diluted 1 to 10 with normal saline. Because of the risk of leakage we programmed the instillation every six hours, with a dwell time of 10 minutes.
After one dressing change we saw a more vital wound bed. After 5 dressing changes the infection was clearly under control and there was a lot of granulation tissue.
In order to simplify the care, and mobilizing the patient, we switched to VAC® therapy.
After 6 dressing changes, the aesthetic surgeon did a wound revision and closed both wounds. After a wound revision with complete wound closure there is a lot of traction on the wound edges. The chance of developing a post- operative seroma or dehiscence is very high. To give the wound a full chance of healing, we installed a Prevena® dressing. We placed an additional strip of Prevena® dressing on the lateral sides of the wound to increase the contact area and to minimize the lateral stress.
The patient was followed by the rheumatologist throughout the admission. He decides when the cortisones could be phased out.
The advantage of the VAC Veraflo® system is that it reaches the entire wound bed by combining negative pressure with instilling a solution. The combination of soaking the solution with intermittent negative pressure therapy gives nice results, even with a complex wound like this.
The advantage of the different applications of negative pressure therapy is that we can use it in different situations, even after revision surgery.
References
- Rycerz M A., Allen D., Lessing C. Supporting negative pressure wound therapy with instillation. International Wound Journal 2013; 10: 20-24
- Back A D, Scheuermann-P C, Willy C. Recommendations on negative pressure wound therapy with instillation and antimicrobial solutions- when, where and how to use: what does the evidence show? International Wound Journal 2013; 10: 32-42.
https://www.nice.org.uk/advice/mib189/chapter/The-technology; The VAC Veraflo® Therapy for infected wounds
3. Grauhan O, Navasardyan A, Hofmann M, et al. J Thorac Cardiovasc Surg 2013; 145: 1387 – 92 World Union of Wound Healing Societies (WUWHS)
4. Masden D, et al. Negative Pressure Wound Therapy for At-Risk Surgical Closures in Patients with Multiple Comorbidities: A Prospective Randomized Controlled Study. Annals of Surgery. 2012 Jun;255(6):1043
5. Christian W. et al. Closed incision negative pressure therapy; international multidisciplinary consensus recommendations. Wound J. 2017; 14:385-398.
6. Consensus Document. Closed surgical incision management: understanding the role of NPWT. Wounds International, 2016)