Case Study
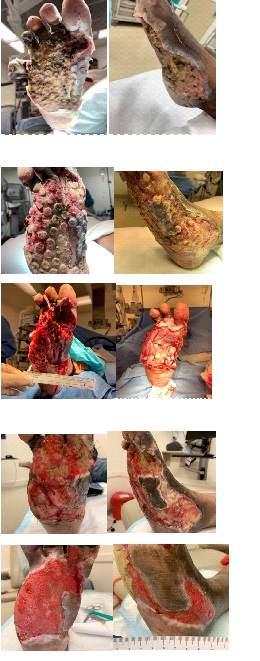
Case Study: DM foot ulcer with osteomyelitis and multiple abscesses resulting in ray amputation- multiple OR debridement I and D
Patient: 60 y/o female admitted to hospital on April ,2019. Her weight, 88.4 kg, height 170 cm, BMI 32.3. PMH: ESRD on dialysis, IDDM, CAD with stents, Hyperlipidemia, DM neuropathy. Patient initially noticed a blister between her right 4th and 5th web space. She initially treated this with antibiotic ointment. When the pain started to increase and noted drainage she presented to the walk in clinic. The x-ray showed underlying signs of osteomyelitis. She was prescribed doxycycline 7 days and to follow up with her Podiatrist.
Patient did not follow up with podiatrist but presents 2 weeks later at the ER with a temp of 38 C. tachycardic and BP 119/90. He foot pain was worsening as well as swelling expanded to bottom 1/3 of right lower leg. Reports fever and chills 3 day.
Diagnosis: Right foot infection.
Initial treatment of therapy:
5/1/2019- OR-Proximal phalangectomy of 5th toe- extensive I and D of multiple abscesses – Antibiotic beads placed.
5/6 –OR- I and D of a plantar access.
5/13- OR extensive I and D of multiple abscess / pulse lavage.
5/15- OR by vascular angiogram. Patient had heparin reaction. Resuscitated.
Unable to get OR clearance to take patient for a foot amputation.
5/16 Verafo started at bedside. To help manage infectious process.
NS 100cc for 2 min cycle every 30 min , 125 mmhg
5/20 dressing change due to leak
5/21 dressing changed due to leak
Changed to Dakins 1/8th strength 20 cc for 5 min cycle every 30 min, 125 mmhg
5/24 obtained OR clearance – Ray amputation 4th and 5th right digits.
OR sharp debridement.
Biologic graft applied with non adherent silicone dressing with vac at 125 mmhg continuous.
6/3 dressing change same settings.
6/5 dressing change with same settings discharged to ECF with vac.
Wound center follows up with Podiatrist
Progress:
Patient continues to epithelialize and wound thickness is now at subcutaneous level. She continues to make weekly progress.
Discharge and follow up: ECF / Wound and center
Patient follows up weekly at wound care center. She was discharged from ECF after completing IV antibiotic management. She continues to be treated with standard NPWV therapy. She received in clinic application of Puraply and Apligraf skin substitute graft.
Economic Value (if applicable):
Below knee amputation avoided. Value priceless.
Clinical outcomes / conclusions:
Veraflow was a critical modality in helping to stop progression of the infection, assisted in removal of bioburden and necrotic tissue and in formation of granulation tissue.
Reference: St Vincent’s Medical Center Bridgeport CT
Dr. Dan Davis DPM
Dr. Denisa Riera DPM
Lea Forcier BSN,RN,CWON