Case Study
Summary
A 59yo female underwent explantation of an infected ileo-femoral bypass with deep femoral vein harvest for reconstruction. This was complicated by a haematoma requiring evacuation. Closure was thus achieved by secondary intention. High dose broad spectrum antibiotic cover created a heavily yeast colonised large thigh wound. V.A.C. Veraflo™ was used for the successful debridement, wound bed preparation and closure of this large thigh wound.
Patient
A 59yo female, presented with an infected ileo-femoral bypass graft. This was explanted and a femoral vein harvest for interposition grafting was performed to maintain perfusion to the limb. Postoperative haematoma formation necessitated evacuation and debridement, resulting in a large thigh wound that subsequently became colonised by yeast, secondary to high dose broad spectrum antibiotic coverage required for treatment of the arterial graft infection.
Medical/Family history
Active smoker
COPD/asthma
IHD
HTN
Diverticular disease
Non-alcoholic fatty liver disease
Obesity
Background
The patient underwent a left ileo-femoral bypass graft for arterial occlusive disease in 2012 using an 8mm Dacron graft.
She returned 6 years later with critical limb ischemia and was treated with implantation of an AFX stent (aorto-bi-iliac unibody stent) for the treatment of aorto-iliac occlusive disease (AIOD).
She then presented with an infected superficial groin collection 3 months later which required incision and drainage. There was felt to be no connection with deeper structures at the time and imaging did not show graft infection at this point. The wound was not primarily closed and healed by secondary intention.
A further 6 months later (9 months post original AFX stent surgery) she re-presented to hospital with a community acquired pneumonia (CAP) requiring ICU admission and a tender left iliac fossa with a PET scan confirming infection of the ileo-femoral graft.
Following ICU stabilisation and recovery from her CAP she underwent limited explantation of the ileo-femoral graft with mobilisation of a sartorial flap. This anastomosis broke down due to residual infection and she underwent complete explantation of the remaining ileo-femoral bypass + AFX stent with reconstruction of the aorto-iliac segment using femoral vein harvested from the thigh. This left a large upper thigh/groin defect which was covered using a rectus flap.
Subsequent to these procedures a large haematoma developed and was evacuated.
This left two large residual open wounds in the groin and upper thigh each with a muscular base, margin of necrotic fat but good skin integrity. Disruption of the venous and lymphatic drainage pathways occurred as a result of the multiple procedures required to successfully and completely remove the infected graft. This caused a highly oedematous and exudative wound.
Prolonged antibiotic use through the 6 months of treatment resulted in colonisation of the thigh wound with a multi-resistant candida parapsilosis complex. Infectious disease consultation was sort throughout the entirety of the treatment course and it was felt that the candida colonisation did not require systemic treatment as it was localised to the wound itself.
Figure 1 illustrates the wound at the completion of all operative procedures at which point intravenous antibiotics and V.A.C.® therapy were instituted for wound management.
Figure 1 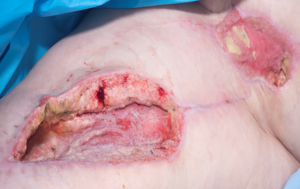
Management
Two defects remained; the groin wound was smaller relative to the thigh wound and was managed with V.A.C.® therapy and then simple dressings. This healed without complication.
For the larger thigh defect, surgical debridement and direct closure of the wound was not felt to be possible in the setting of yeast colonisation, as such non-operative wound management strategies were sort.
Initial treatment of the wound with a total of 4 weeks of V.A.C.® therapy and intravenous antibiotics resulted in heavy colonisation of the wound base with yeast. The standard V.A.C.® therapy coupled with the highly exudative wound was felt to have created a warm closed environment enabling the proliferation of the yeast organism.
As such V.A.C. Veraflo™ Therapy with Prontosan®, a combination antiseptic (Polyhexamethylene Biguanide) and surfactant (betaine), was employed in an attempt to remove the yeast film that developed on the wound preventing closure. An initial 2 week period of V.A.C. Veraflo™ Therapy and Prontosan® instillation was successful in positioning the wound for conversion to standard V.A.C.® therapy and the patient was then discharged into the community.
Unfortunately, the patient experienced further tissue necrosis in the thigh wound, believed to be secondary to the rampant candida infection which again flourished in the warm conditions of the standard V.A.C.® therapy.
The patient was readmitted and V.A.C. Veraflo™ with Prontosan® was again initiated with poor response. Figure 2 shows increased yeast burden following treatment with V.A.C. Veraflo™ Therapy with Prontosan® instillation and dwell.
Figure 2 
The VA.C. Veraflo™ was ceased and a regime of potassium permanganate soaks applied twice daily was employed in an effort to dry the wound and curtail the yeast colonisation. After 4 days of daily treatment this achieved stasis but no improvement in the wound, and wound exudate was difficult to manage with the cessation of the V.A.C.® Figure 3 depicts the result of this therapy.
Figure 3 
V.A.C. Veraflo™ Therapy was re-employed to manage the highly exudative component of the wound and Microdacyn® was initiated as the instillation solution. Microdacyn® is a superoxidised solution that increases the permeability of cell wall in single cell organism thus causing them to disintegrate. As such it is effective in the debridement of yeast colonisation. Microdacyn® was instilled in 5 hourly cycles for a total of 10 minutes dwell time each cycle. V.A.C. Veraflo™ and Microdacyn® instillation and dwell as employed for a total of 2 weeks (5 cycles/dressing changes).
Outcome
The combination of V.A.C. Veraflo™ Therapy with Microdacyn® instillation and dwell resulted in resolution of the yeast burden with interval reduction in the size of the wound which allowed for surgical debridement and partial closure. Figure 4 depicts interval improvement in the yeast burden. A return to the V.A.C. Veraflo™ system also assisted in managing the significant lymphoedema/oedema in the local wound area and proximal limb, through negative pressure splinting of the wound and management of chronic wound exudate.
Figure 4 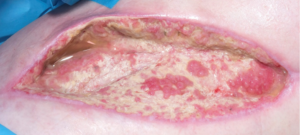
With the candida infection managed and the wound bed significantly improved, the wound bed was debrided and a split skin graft was placed insitu in the groin wound.
The patient has continued to progress to complete wound healing, Figure 5 depicts her wound several weeks prior to achieving complete epithelialisation of her significant thigh wound.
Figure 5 
Reference
Flinders Medical Centre, SALHN, Bedford Park, South Australia. Dr Phillip Puckridge, Consultant Vascular Surgeon, Head of Unit, Dept. Vascular and Endovascular Surgery